Ulcerative colitis (UC) is a chronic inflammatory bowel disease (IBD) that primarily affects the colon and rectum. It causes inflammation, ulcers, and sores in the lining of the large intestine, leading to symptoms such as abdominal pain, diarrhea, and rectal bleeding. Ulcerative colitis can significantly impact a person’s quality of life, requiring ongoing medical management. While there is no cure, various treatments can help manage symptoms and induce remission. In this comprehensive guide, we will explore the types, causes, symptoms, prevention, diagnosis, and treatment of ulcerative colitis.
Types of Ulcerative Colitis
Ulcerative colitis is categorized based on the location and extent of inflammation in the colon. The primary types include:
1. Ulcerative Proctitis
Ulcerative proctitis is the mildest form of ulcerative colitis, where inflammation is limited to the rectum. Common symptoms include rectal bleeding, urgency to pass stool, and rectal pain. Since the inflammation does not extend beyond the rectum, individuals with ulcerative proctitis may not experience severe abdominal pain or diarrhea. Treatment typically involves topical medications such as mesalamine suppositories or corticosteroids.
2. Proctosigmoiditis
This type of UC affects the rectum and the sigmoid colon (the lower part of the colon). Symptoms include bloody diarrhea, cramps, and an urgency to defecate. Some individuals may also experience tenesmus, a feeling of incomplete bowel evacuation. The inflammation in proctosigmoiditis is more extensive than ulcerative proctitis but does not affect the entire colon. Treatment often involves aminosalicylates, corticosteroids, and immunosuppressants in severe cases.
3. Left-Sided Colitis
Left-sided colitis, also known as distal colitis, involves inflammation extending from the rectum up to the descending colon. Symptoms include abdominal cramping on the left side, bloody diarrhea, weight loss, and decreased appetite. Because the inflammation covers a larger portion of the colon, symptoms are more intense than in proctosigmoiditis. Treatment usually involves oral medications like mesalamine, corticosteroids, or biologics to reduce inflammation and manage symptoms.
4. Pancolitis
Pancolitis, also called extensive colitis, affects the entire colon. It is one of the more severe forms of UC and is associated with frequent, severe diarrhea, significant weight loss, fatigue, and abdominal pain. Patients with pancolitis have a higher risk of developing complications such as anemia, dehydration, and colon cancer if left untreated. Treatment typically includes a combination of oral and intravenous medications, such as biologics, immunosuppressants, and corticosteroids. In some cases, surgery may be required if medications fail to control the condition.
5. Fulminant Colitis
Fulminant colitis is the most severe and life-threatening form of ulcerative colitis. It is a rare but dangerous condition characterized by severe diarrhea, fever, dehydration, severe abdominal pain, and potential toxic megacolon (a condition where the colon becomes significantly enlarged). Patients with fulminant colitis often require hospitalization, intravenous fluids, high-dose steroids, and sometimes emergency surgery to remove the colon (colectomy) if complications arise.

Symptoms of Ulcerative Colitis
Symptoms of UC vary in severity and may come and go, with periods of remission and flare-ups. Common symptoms include:
1. Gastrointestinal Symptoms
- Persistent diarrhea with blood or pus
- Abdominal pain and cramping
- Rectal bleeding and urgency
- Tenesmus (a constant urge to pass stool)
- Bloating and gas
2. Systemic Symptoms
- Fatigue and weakness
- Fever during flare-ups
- Weight loss
- Loss of appetite
3. Extraintestinal Symptoms
Ulcerative colitis can affect other parts of the body, leading to:
- Joint pain and swelling (arthritis)
- Skin rashes and ulcers
- Eye inflammation (uveitis or episcleritis)
- Liver problems
Prevention of Ulcerative Colitis
While ulcerative colitis cannot always be prevented, certain lifestyle changes may reduce the risk of flare-ups and complications.
1. Maintain a Healthy Diet
- Eat fiber-rich foods to support gut health
- Avoid processed foods, alcohol, and excessive caffeine
- Stay hydrated to prevent dehydration from diarrhea
2. Manage Stress
- Practice mindfulness, yoga, or meditation
- Engage in regular physical activity
- Seek therapy or counseling if needed
3. Avoid Smoking
Smoking can increase the severity of UC symptoms and contribute to complications.
4. Limit Use of NSAIDs
Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen may trigger UC flare-ups.
Diagnosis of Ulcerative Colitis
Ulcerative colitis (UC) is a chronic inflammatory bowel disease that requires an accurate diagnosis to ensure effective treatment. Because UC shares symptoms with other gastrointestinal disorders, a comprehensive diagnostic approach is necessary. The process typically involves a combination of clinical evaluation, laboratory tests, imaging studies, and endoscopic procedures. Here is a detailed look at the primary methods used for diagnosing ulcerative colitis:
Medical History and Physical Examination
A doctor will begin by gathering a thorough medical history, including the patient’s symptoms, their duration, family history of inflammatory bowel diseases, and lifestyle factors that may contribute to gastrointestinal issues. Common symptoms of UC include persistent diarrhea, abdominal pain, rectal bleeding, and weight loss. During the physical examination, the doctor may check for signs of tenderness in the abdominal area and look for other symptoms such as fever, anemia, or dehydration.
Laboratory Tests
Several blood and stool tests are conducted to help differentiate ulcerative colitis from other conditions:
- Blood Tests: These tests assess overall health and look for signs of inflammation or complications. Key blood tests include:
- Complete Blood Count (CBC): This test checks for anemia, which can result from chronic blood loss due to UC.
- C-reactive Protein (CRP) and Erythrocyte Sedimentation Rate (ESR): These inflammation markers help determine the severity of the disease.
- Electrolyte and Liver Function Tests: UC can affect nutrient absorption, so these tests evaluate hydration and organ function.
- Stool Tests: A stool sample helps rule out infections and detect the presence of inflammatory markers such as calprotectin and lactoferrin. A stool culture may be performed to check for bacterial, viral, or parasitic infections that can mimic UC symptoms.
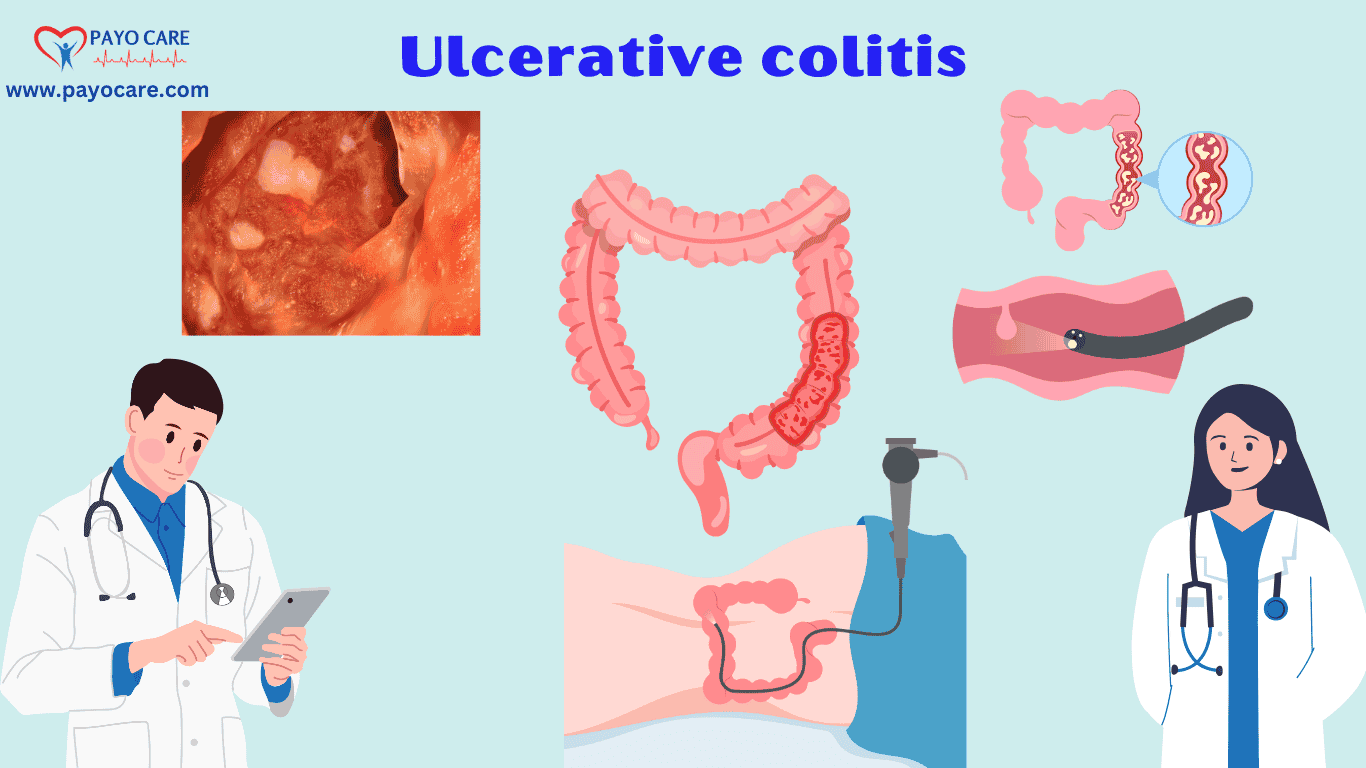
Endoscopic Procedures
Endoscopy plays a crucial role in confirming the diagnosis of ulcerative colitis by allowing direct visualization of the colon:
- Colonoscopy with Biopsy: A colonoscopy is the most definitive test for UC. During this procedure, a flexible tube with a camera is inserted into the colon to examine inflammation and ulcerations. Biopsy samples are collected from the colon lining to look for characteristic changes associated with UC.
- Flexible Sigmoidoscopy: If a full colonoscopy is not required, a sigmoidoscopy can be performed to examine the rectum and lower colon. This is a quicker and less invasive procedure but may not provide a complete picture of the disease.
Imaging Studies
Imaging tests help assess the extent of inflammation and rule out complications such as bowel obstruction or perforation:
- Abdominal X-ray: Used in severe cases to check for toxic megacolon, a life-threatening complication of UC.
- CT Scan or MRI: These imaging techniques provide detailed images of the digestive tract and help identify complications beyond the colon.

Treatment of Ulcerative Colitis
While there is no cure for UC, treatments help manage symptoms and induce remission.
1. Medications
- Aminosalicylates (5-ASAs): Reduce inflammation (e.g., mesalamine, sulfasalazine).
- Corticosteroids: Used for short-term relief during flare-ups.
- Immunosuppressants: Suppress immune activity (e.g., azathioprine, methotrexate).
- Biologics: Target specific immune system proteins (e.g., infliximab, adalimumab).
- JAK Inhibitors: (e.g., tofacitinib) used in severe cases.
2. Lifestyle and Dietary Changes
- Eat smaller meals more frequently
- Keep a food journal to track triggers
- Consider probiotics for gut health
3. Surgery
In severe cases, surgery may be necessary, such as:
- Proctocolectomy: Removal of the entire colon and rectum
- Ileal Pouch-Anal Anastomosis (J-pouch surgery): Creates a new way for stool to exit the body
4. Alternative Therapies
- Acupuncture, herbal supplements, and stress-reducing techniques may complement medical treatment.
Key Points
- Ulcerative colitis types
- Causes of ulcerative colitis
- Symptoms of ulcerative colitis
- Ulcerative colitis prevention
- How to diagnose ulcerative colitis
- Ulcerative colitis treatment options
- Best diet for ulcerative colitis
- Inflammatory bowel disease (IBD)
- Ulcerative colitis medications
- Biologics for ulcerative colitis
- Ulcerative colitis vs Crohn’s disease
- Ulcerative proctitis symptoms
- Pancolitis treatment options
- Colonoscopy for ulcerative colitis
- Surgery for ulcerative colitis
- Natural remedies for ulcerative colitis
- Ulcerative colitis flare-up management
- Foods to avoid with ulcerative colitis
- Immunosuppressants for ulcerative colitis
- Long-term effects of ulcerative colitis
Frequently Asked Questions
1. What is Ulcerative Colitis?
Ulcerative Colitis (UC) is a chronic inflammatory bowel disease (IBD) that causes inflammation and ulcers in the colon and rectum, leading to symptoms like diarrhea, abdominal pain, and rectal bleeding.
2. What causes Ulcerative Colitis?
The exact cause is unknown, but factors like immune system dysfunction, genetics, environmental triggers, and gut microbiome imbalance may contribute to its development.
3. What are the early symptoms of Ulcerative Colitis?
Common early symptoms include frequent diarrhea, abdominal cramps, rectal bleeding, fatigue, and an urgent need to use the bathroom.
4. How is Ulcerative Colitis diagnosed?
Doctors diagnose UC using blood tests, stool tests, colonoscopy, CT scans, or MRI scans to assess inflammation and rule out other conditions.
5. Can Ulcerative Colitis be cured?
There is no permanent cure for UC, but medications, dietary changes, and in severe cases, surgery can help manage symptoms and improve quality of life.
6. What foods should be avoided with Ulcerative Colitis?
People with UC should avoid dairy, high-fiber foods, spicy foods, carbonated drinks, caffeine, alcohol, and processed foods that can trigger flare-ups.
7. Is Ulcerative Colitis a life-threatening disease?
UC is not usually life-threatening, but severe cases can lead to complications like colon perforation, toxic megacolon, or an increased risk of colon cancer if left untreated.
8. Can stress trigger Ulcerative Colitis flare-ups?
Yes, stress does not cause UC, but it can worsen symptoms and trigger flare-ups, making stress management important in disease control.
9. What are the treatment options for Ulcerative Colitis?
Treatment options include anti-inflammatory drugs, immunosuppressants, biologics, lifestyle changes, and in severe cases, surgery such as a colectomy.
10. Can Ulcerative Colitis affect other parts of the body?
Yes, UC can cause complications outside the digestive system, including joint pain, eye inflammation, skin disorders, and liver issues.
Conclusion
Ulcerative colitis is a chronic condition that requires lifelong management. While it can be challenging, early diagnosis and appropriate treatment can improve quality of life. Patients should work closely with healthcare providers to develop a personalized management plan. Lifestyle changes, medications, and, in some cases, surgery can help control symptoms and maintain remission. By staying informed and proactive, individuals with ulcerative colitis can lead fulfilling lives despite their diagnosis.