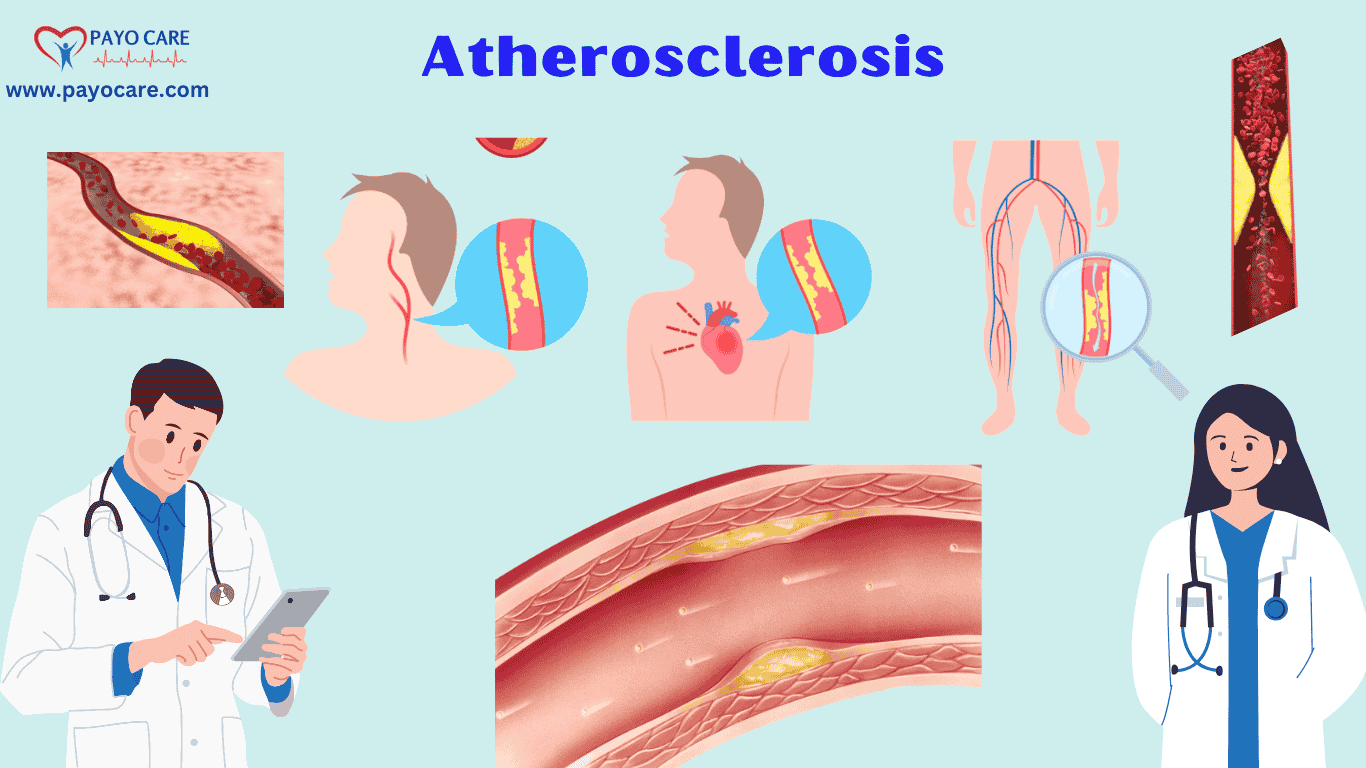
Atherosclerosis is a chronic condition in which arteries become narrowed and hardened due to the buildup of plaque—a combination of fat, cholesterol, and other substances—on the artery walls. Over time, this plaque buildup can restrict blood flow, leading to serious complications such as heart attacks, strokes, and peripheral artery disease.
Atherosclerosis often develops silently over decades, making early detection and prevention crucial. Understanding the different types, causes, symptoms, and treatment options can help individuals take proactive measures to protect their cardiovascular health. This article provides a comprehensive overview of atherosclerosis, including its types, causes, symptoms, prevention, risk factors, diagnosis, treatment, and when to seek medical attention.
Types of Atherosclerosis
Atherosclerosis can affect different arteries throughout the body, leading to various types, including:
1. Coronary Atherosclerosis
Coronary atherosclerosis affects the coronary arteries, which supply blood to the heart. When plaque builds up in these arteries, it can lead to reduced blood flow, causing chest pain (angina) and increasing the risk of heart attacks. In severe cases, complete blockage of the arteries can result in myocardial infarction (heart attack). Treatment includes lifestyle changes, medications like statins and blood thinners, and in some cases, surgical interventions like angioplasty or bypass surgery.
2. Cerebral Atherosclerosis
Cerebral atherosclerosis occurs in the arteries supplying blood to the brain. Plaque buildup in these arteries can lead to reduced blood flow, increasing the risk of stroke or transient ischemic attacks (mini-strokes). Symptoms may include dizziness, difficulty speaking, vision problems, and weakness on one side of the body. Management includes controlling risk factors like high blood pressure, cholesterol levels, and diabetes through medications and lifestyle modifications.
3. Peripheral Arterial Atherosclerosis
This type affects the arteries that supply blood to the limbs, particularly the legs. It can lead to peripheral artery disease (PAD), characterized by pain or cramping in the legs during physical activity (claudication), numbness, or cold extremities. Severe cases may result in non-healing wounds or even gangrene, potentially requiring amputation. Treatment involves medications, exercise programs, and surgical procedures like angioplasty or bypass grafting to restore blood flow.
4. Aortic Atherosclerosis
Aortic atherosclerosis affects the aorta, the body’s largest artery that carries blood from the heart to the rest of the body. Plaque buildup in the aorta can weaken the artery wall, increasing the risk of aneurysms (bulging of the artery) or dissections (tears in the artery wall), which can be life-threatening. Symptoms may not appear until complications arise, requiring medical imaging for early detection. Treatment involves managing cholesterol, blood pressure, and in severe cases, surgical repair of aneurysms.
5. Renal Atherosclerosis
Renal atherosclerosis affects the arteries supplying blood to the kidneys, potentially leading to chronic kidney disease or hypertension. When blood flow to the kidneys is restricted, they may not function properly, causing fluid retention and increased blood pressure. Symptoms may include high blood pressure that does not respond to medication and signs of kidney dysfunction. Treatment includes blood pressure management, cholesterol-lowering drugs, and in severe cases, stenting or bypass surgery.
Causes of Atherosclerosis
Atherosclerosis is primarily caused by damage to the inner lining of arteries (endothelium), which triggers inflammation and plaque buildup. The main causes include:
1. High Cholesterol Levels
- LDL Cholesterol (“Bad” Cholesterol): Excess low-density lipoprotein (LDL) cholesterol accumulates in artery walls, forming plaques.
- Low HDL Cholesterol (“Good” Cholesterol): High-density lipoprotein (HDL) helps remove LDL cholesterol from the arteries, so low levels contribute to plaque buildup.
2. High Blood Pressure (Hypertension)
- Persistent high blood pressure damages artery walls, making them more prone to plaque accumulation.
- Increases the risk of artery narrowing and rupture.
3. Smoking and Tobacco Use
- Chemicals in tobacco damage blood vessels and promote plaque formation.
- Reduces oxygen supply to tissues and increases blood clot risk.
4. Diabetes and Insulin Resistance
- High blood sugar damages blood vessels and accelerates plaque buildup.
- Diabetics have a higher risk of developing atherosclerosis at an earlier age.
5. Obesity and Poor Diet
- Excess body weight contributes to high cholesterol, high blood pressure, and diabetes, all of which increase atherosclerosis risk.
- Diets high in trans fats, saturated fats, and refined sugars promote plaque formation.
6. Sedentary Lifestyle
- Lack of physical activity leads to weight gain, high blood pressure, and poor circulation.
- Exercise helps maintain healthy cholesterol levels and arterial flexibility.
7. Chronic Inflammation
- Conditions like rheumatoid arthritis, lupus, and chronic infections trigger inflammation that can damage arteries.
- C-reactive protein (CRP), an inflammation marker, is often elevated in individuals with atherosclerosis.
8. Genetic Factors and Family History
- A family history of heart disease increases the risk of early-onset atherosclerosis.
- Some individuals inherit a predisposition to high cholesterol and blood pressure.
9. Excessive Alcohol Consumption
- Heavy drinking raises blood pressure and triglyceride levels, increasing plaque buildup.
- Moderate alcohol consumption may have some heart benefits, but excessive intake is harmful.
10. Aging
- As people age, arteries naturally lose flexibility and are more prone to plaque buildup.
- Risk increases significantly after age 45 in men and after menopause in women.

Symptoms of Atherosclerosis
Atherosclerosis often develops silently and may not cause symptoms until an artery is significantly narrowed or blocked. The symptoms vary based on which arteries are affected:
1. Coronary Artery Disease Symptoms
- Chest pain or pressure (angina)
- Shortness of breath
- Fatigue
- Heart palpitations
2. Carotid Artery Disease Symptoms
- Sudden weakness or numbness in the face, arms, or legs
- Difficulty speaking or understanding speech
- Blurred vision or vision loss
- Dizziness or loss of balance (signs of a stroke or transient ischemic attack)
3. Peripheral Artery Disease Symptoms
- Leg pain, cramping, or weakness, especially while walking (claudication)
- Coldness or numbness in the legs or feet
- Slow-healing sores or ulcers on the feet or toes
4. Renal Artery Disease Symptoms
- High blood pressure that is difficult to control
- Kidney dysfunction or failure
5. Aortic Atherosclerosis Symptoms
- Aneurysm formation, which may cause back or abdominal pain
- Risk of life-threatening rupture
Prevention of Atherosclerosis
Preventing atherosclerosis requires long-term lifestyle changes to reduce risk factors and maintain healthy arteries.
1. Maintain a Healthy Diet
A heart-healthy diet helps in reducing cholesterol levels and preventing plaque buildup in the arteries. To prevent atherosclerosis:
- Eat fiber-rich foods: Whole grains, fruits, and vegetables help lower bad cholesterol (LDL) and improve heart health.
- Consume healthy fats: Opt for unsaturated fats found in nuts, seeds, olive oil, and fatty fish instead of trans and saturated fats.
- Reduce sugar and refined carbs: High sugar intake contributes to obesity and insulin resistance, increasing atherosclerosis risk.
- Limit sodium intake: Excess salt can raise blood pressure, increasing strain on arteries.
2. Engage in Regular Physical Activity
Exercise strengthens the heart and improves circulation, reducing the risk of plaque buildup. To maintain heart health:
- Aim for at least 150 minutes of moderate exercise or 75 minutes of vigorous exercise weekly.
- Include activities like walking, jogging, cycling, and swimming.
- Strength training at least twice a week helps maintain overall cardiovascular fitness.
3. Maintain a Healthy Weight
Being overweight or obese increases the risk of high cholesterol, diabetes, and hypertension, which contribute to atherosclerosis. To manage weight effectively:
- Follow a balanced diet with portion control.
- Engage in regular physical activity.
- Seek professional guidance if needed for weight management.
4. Quit Smoking and Limit Alcohol
Smoking damages artery walls, increases plaque buildup, and reduces oxygen levels in the blood. To reduce your risk:
- Seek support to quit smoking through counseling, medications, or nicotine replacement therapy.
- Limit alcohol consumption to moderate levels (one drink per day for women, two for men).
5. Manage Stress Levels
Chronic stress can contribute to high blood pressure and unhealthy lifestyle habits that increase the risk of atherosclerosis. To manage stress effectively:
- Practice relaxation techniques such as meditation, deep breathing, and yoga.
- Engage in hobbies and social activities to reduce anxiety.
- Ensure adequate sleep for overall well-being.
6. Monitor and Control Health Conditions
High blood pressure, high cholesterol, and diabetes are major risk factors for atherosclerosis. To manage these conditions:
- Regularly monitor blood pressure and cholesterol levels.
- Follow prescribed medications and lifestyle recommendations from healthcare professionals.
- Maintain stable blood sugar levels through diet and exercise if you have diabetes.
7. Regular Medical Check-Ups
Early detection and management of cardiovascular risk factors can prevent complications of atherosclerosis. Consult a doctor if you experience symptoms such as chest pain, shortness of breath, or fatigue. Regular screenings can help detect and manage risk factors effectively.
1. Medical History and Physical Examination
A doctor will begin by assessing the patient’s medical history, lifestyle, and risk factors, including:
- Family history of heart disease or stroke
- Smoking, alcohol consumption, and dietary habits
- Presence of conditions like diabetes, high blood pressure, or high cholesterol
- Symptoms such as chest pain, shortness of breath, leg pain, or dizziness
During a physical examination, the doctor may check for:
- Blood pressure levels (to detect hypertension)
- Pulse strength (weak pulses may indicate reduced blood flow)
- Bruit sounds (abnormal artery sounds due to turbulent blood flow)
- Skin color changes or ulcers (signs of poor circulation in the legs)
2. Laboratory Tests
A. Blood Tests
-
Lipid Profile Test
- Measures levels of cholesterol and triglycerides in the blood.
- High LDL (“bad” cholesterol) and low HDL (“good” cholesterol) indicate increased risk.
-
High-Sensitivity C-Reactive Protein (hs-CRP) Test
- Detects inflammation in blood vessels, which is associated with atherosclerosis.
-
Blood Sugar (Glucose) and HbA1c Tests
- Assesses diabetes risk, a major contributor to atherosclerosis.
-
Homocysteine Test
- High levels of homocysteine can damage arteries and increase heart disease risk.
3. Imaging and Diagnostic Tests
A. Non-Invasive Tests
-
Electrocardiogram (ECG or EKG)
- Detects abnormal heart rhythms or signs of past heart attacks.
-
Echocardiogram
- Uses ultrasound waves to check heart function and detect reduced blood flow.
-
Ankle-Brachial Index (ABI)
- Compares blood pressure in the arms and legs to identify peripheral artery disease (PAD).
-
Carotid Ultrasound
- Uses sound waves to assess blood flow and detect plaque buildup in the carotid arteries.
-
Coronary Calcium Scan (CT Calcium Score)
- A CT scan that measures calcium deposits in coronary arteries, indicating plaque buildup.
-
Magnetic Resonance Angiography (MRA) or CT Angiography
- Provides detailed images of arteries to detect blockages.
B. Invasive Tests
-
Coronary Angiography (Cardiac Catheterization)
- A catheter is inserted into an artery and contrast dye is injected to visualize blockages using X-rays.
- Used in severe cases to assess the need for stents or bypass surgery.
-
Intravascular Ultrasound (IVUS)
- A small ultrasound probe is inserted into the artery to assess plaque buildup more precisely.
4. Differential Diagnosis
Atherosclerosis symptoms can resemble other conditions, including:
- Angina (chest pain due to other causes like muscle strain)
- Blood clot disorders
- Aortic aneurysm
- Heart valve diseases

Treatment of Atherosclerosis
Treatment focuses on slowing disease progression, managing symptoms, and preventing complications.
1. Medications
- Statins: Lower cholesterol levels (e.g., atorvastatin, rosuvastatin).
- Blood Pressure Medications: Control hypertension (e.g., ACE inhibitors, beta-blockers).
- Blood Thinners: Reduce clot risk (e.g., aspirin, clopidogrel).
2. Lifestyle Modifications
- Essential for long-term management and prevention.
3. Surgical Procedures
- Angioplasty and Stenting: Opens narrowed arteries using a balloon and stent.
- Bypass Surgery: Creates a detour around blocked arteries.
When to See a Doctor
Seek medical attention if you experience:
- Chest pain or tightness
- Sudden weakness or difficulty speaking (possible stroke)
- Severe leg pain or non-healing wounds
- Uncontrolled high blood pressure or diabetes
Emergency Symptoms
- Symptoms of a heart attack (severe chest pain, shortness of breath, nausea)
- Stroke warning signs (sudden numbness, confusion, or loss of coordination)
Key points
- What is atherosclerosis?
- Causes of atherosclerosis
- Symptoms of atherosclerosis
- Types of atherosclerosis
- How to prevent atherosclerosis
- Diagnosis of atherosclerosis
- Treatment for atherosclerosis
- Best diet for atherosclerosis prevention
- Medications for atherosclerosis
- Atherosclerosis vs arteriosclerosis
- Can atherosclerosis be reversed?
- Risk factors for atherosclerosis
- How does atherosclerosis affect the heart?
- Coronary artery disease and atherosclerosis
- Peripheral artery disease symptoms
- Lifestyle changes for atherosclerosis
- Atherosclerosis and high cholesterol
- Natural remedies for atherosclerosis
- Surgical treatment for atherosclerosis
- Early signs of atherosclerosis
10 FAQs on Atherosclerosis
1. What is atherosclerosis?
Atherosclerosis is a condition where fatty deposits (plaques) build up inside the arteries, causing them to narrow and harden, restricting blood flow and increasing the risk of heart disease and stroke.
2. What causes atherosclerosis?
The main causes include high cholesterol, high blood pressure, smoking, diabetes, obesity, poor diet, lack of exercise, and genetic factors.
3. What are the early symptoms of atherosclerosis?
Early stages may not show symptoms, but as arteries narrow, symptoms like chest pain (angina), shortness of breath, fatigue, numbness in limbs, or high blood pressure may appear.
4. How is atherosclerosis diagnosed?
Doctors use blood tests, angiography, ultrasound, CT scans, MRIs, and the ankle-brachial index (ABI) test to check for artery narrowing and blockages.
5. Can atherosclerosis be prevented?
Yes, by maintaining a healthy diet, exercising regularly, quitting smoking, managing blood pressure and cholesterol levels, and controlling diabetes.
6. What is the best treatment for atherosclerosis?
Treatment includes lifestyle changes, medications (statins, blood pressure drugs, antiplatelets), and in severe cases, surgical procedures like angioplasty, stent placement, or bypass surgery.
7. Is atherosclerosis reversible?
While plaque buildup cannot be completely removed, lifestyle changes and medications can slow, stop, or even slightly reverse the progression of the disease.
8. What is the difference between atherosclerosis and arteriosclerosis?
Atherosclerosis refers to plaque buildup in the arteries, while arteriosclerosis is a broader term for artery hardening due to aging and other factors.
9. Can atherosclerosis lead to serious complications?
Yes, it can cause heart attacks, strokes, aneurysms, peripheral artery disease, kidney disease, and other life-threatening conditions if left untreated.
10. When should I see a doctor for atherosclerosis?
You should see a doctor if you experience symptoms like chest pain, shortness of breath, leg pain while walking, high blood pressure, or a family history of heart disease.
Conclusion
Atherosclerosis is a serious but manageable condition. Early detection, lifestyle changes, and appropriate medical intervention can significantly reduce complications. Regular health check-ups and proactive measures can help maintain a healthy cardiovascular system.
Note:This is only for informational purposes