Rheumatoid arthritis (RA) is a chronic autoimmune disorder that primarily affects the joints, causing inflammation, pain, and eventual joint damage. Unlike osteoarthritis, which results from wear and tear, RA occurs when the immune system mistakenly attacks the body’s own tissues, particularly the synovium (the lining of the membranes that surround the joints). This article provides a comprehensive overview of rheumatoid arthritis, including its types, causes, symptoms, prevention strategies, risk factors, diagnosis, treatment options, and when to seek medical attention.
Types of Rheumatoid Arthritis
Rheumatoid arthritis is not a one-size-fits-all condition. It can manifest in different ways, and understanding its types can help in managing the disease effectively.
1. Seropositive Rheumatoid Arthritis
Seropositive RA is the most common type and occurs when a person tests positive for rheumatoid factor (RF) or anti-cyclic citrullinated peptide (anti-CCP) antibodies. These antibodies attack healthy joint tissues, leading to chronic inflammation. Symptoms include joint pain, swelling, stiffness (especially in the morning), and fatigue. Seropositive RA is often more severe and may involve extra-articular complications such as lung or cardiovascular disease. Treatment includes disease-modifying antirheumatic drugs (DMARDs), biologics, and lifestyle changes.
2. Seronegative Rheumatoid Arthritis
Seronegative RA occurs when a person has rheumatoid arthritis symptoms but does not test positive for RF or anti-CCP antibodies. The symptoms and progression of seronegative RA can be similar to seropositive RA, but it may be less severe in some cases. Over time, some seronegative patients may develop detectable autoantibodies. Treatment is similar to seropositive RA and includes DMARDs, biologics, and physical therapy.
3. Juvenile Rheumatoid Arthritis (JRA) / Juvenile Idiopathic Arthritis (JIA)
Juvenile rheumatoid arthritis, also known as juvenile idiopathic arthritis (JIA), affects children under the age of 16. It is an autoimmune condition that leads to joint pain, swelling, stiffness, and potential growth issues. There are several subtypes of JIA, including oligoarticular, polyarticular, and systemic JIA, each with different symptoms and levels of severity. Treatment includes NSAIDs, corticosteroids, DMARDs, and physical therapy to manage inflammation and preserve joint function.
4. Palindromic Rheumatism
Palindromic rheumatism is a rare type of rheumatoid arthritis characterized by episodic flare-ups of joint pain and swelling that resolve without causing permanent joint damage. These episodes can last from a few hours to several days. Some individuals with palindromic rheumatism may eventually develop full-blown RA. Treatment focuses on managing flare-ups with NSAIDs, corticosteroids, and DMARDs to prevent disease progression.
5. Felty’s Syndrome
Felty’s syndrome is a rare but severe form of RA that includes an enlarged spleen (splenomegaly) and a reduced white blood cell count (neutropenia), which increases the risk of infections. It primarily affects individuals with long-standing, severe seropositive RA. Symptoms include recurrent infections, severe fatigue, and leg ulcers. Treatment involves aggressive RA management with DMARDs, biologics, and sometimes splenectomy in extreme cases.
6. Rheumatoid Vasculitis (RV)
Rheumatoid vasculitis is a rare and serious complication of long-term RA, affecting the blood vessels and leading to tissue damage. It can cause skin ulcers, neuropathy, and organ damage in severe cases. Treatment involves immunosuppressive medications like corticosteroids and DMARDs to control inflammation and prevent complications
Causes of Rheumatoid Arthritis
The exact cause of RA remains unknown, but it is believed to result from a combination of genetic, environmental, and immunological factors.
a. Genetic Factors
- Certain genes, such as HLA-DR4, are associated with an increased risk of developing RA.
- Family history of RA or other autoimmune diseases can predispose individuals to the condition.
b. Environmental Triggers
- Infections: Viral or bacterial infections may trigger RA in genetically susceptible individuals.
- Smoking: A significant risk factor, especially in those with a genetic predisposition.
- Hormonal Changes: Women are more likely to develop RA, suggesting a role for hormones like estrogen.
c. Immune System Dysfunction
- In RA, the immune system mistakenly attacks the synovium, leading to inflammation and joint damage.
- Autoantibodies like RF and anti-CCP play a key role in this process.
3. Symptoms of Rheumatoid Arthritis
RA symptoms can vary in severity and may come and go in periods known as flares. Common symptoms include:
a. Joint Symptoms
- Pain: Persistent pain in the affected joints, often worse in the morning or after periods of inactivity.
- Swelling: Inflammation causes the joints to become swollen and tender.
- Stiffness: Morning stiffness lasting more than 30 minutes is a hallmark of RA.
- Redness and Warmth: Inflamed joints may appear red and feel warm to the touch.
b. Systemic Symptoms
- Fatigue: A common and often debilitating symptom.
- Fever: Low-grade fever may accompany flares.
- Weight Loss: Unintended weight loss can occur due to chronic inflammation.
c. Extra-Articular Manifestations
- Rheumatoid Nodules: Firm lumps under the skin, often near joints.
- Eye Problems: Dryness, redness, or pain due to inflammation.
- Lung Involvement: Inflammation of the lung tissue or lining.
- Cardiovascular Issues: Increased risk of heart disease and stroke.

Prevention of Rheumatoid Arthritis
While RA cannot be entirely prevented, certain lifestyle changes may reduce the risk or delay its onset:
1. Maintain a Healthy Diet
A well-balanced diet can help reduce inflammation and support joint health. To prevent rheumatoid arthritis:
- Eat anti-inflammatory foods: Include fatty fish, nuts, seeds, olive oil, and leafy greens, which contain omega-3 fatty acids and antioxidants.
- Increase fiber intake: Whole grains, fruits, and vegetables support gut health and help regulate inflammation.
- Avoid processed foods: Sugary snacks, refined carbohydrates, and trans fats can increase inflammation and contribute to weight gain.
- Limit red meat and dairy: Some studies suggest that reducing red meat and dairy intake may help lower inflammation levels.
2. Engage in Regular Physical Activity
Regular exercise helps maintain joint flexibility and reduces inflammation. To support joint health:
- Aim for at least 150 minutes of moderate exercise per week, such as walking, swimming, or cycling.
- Incorporate strength training to support muscle health and joint stability.
- Practice low-impact exercises like yoga and stretching to improve flexibility and reduce stiffness.
3. Maintain a Healthy Weight
Excess body weight puts additional strain on the joints and increases inflammation. To manage weight effectively:
- Follow a balanced diet with portion control.
- Engage in regular physical activity to maintain a healthy weight.
- Seek professional guidance for weight management if needed.
4. Avoid Smoking and Limit Alcohol
Smoking is a significant risk factor for rheumatoid arthritis, as it increases inflammation and weakens the immune system. To lower your risk:
- Quit smoking with the help of counseling, medications, or nicotine replacement therapy.
- Limit alcohol intake, as excessive consumption can lead to inflammation and weaken the immune response.
5. Manage Stress Levels
Chronic stress can trigger inflammation and negatively impact the immune system, increasing the risk of RA. To manage stress effectively:
- Practice relaxation techniques such as meditation, deep breathing, and yoga.
- Engage in hobbies and social activities to reduce anxiety and improve mental well-being.
- Ensure adequate sleep to support immune function and reduce inflammation.
6. Protect Your Joints
Reducing strain on the joints can help prevent long-term damage. To maintain joint health:
- Use proper body mechanics when lifting heavy objects to avoid joint stress.
- Avoid repetitive motions that can lead to joint overuse and injury.
- Wear supportive footwear to reduce pressure on weight-bearing joints.
7. Regular Medical Check-Ups
Early detection and management of risk factors can help prevent complications associated with RA. To monitor joint health:
- Consult a doctor if you experience persistent joint pain, stiffness, or swelling.
- Regular screenings and blood tests can help detect early signs of autoimmune activity.
- Follow medical advice and take prescribed medications if you have an increased risk of developing RA.
Risk Factors for Rheumatoid Arthritis
Several factors increase the likelihood of developing RA:
a. Age
- RA can occur at any age but is most commonly diagnosed between 30 and 60.
b. Gender
- Women are two to three times more likely to develop RA than men.
c. Family History
- A family history of RA or other autoimmune diseases increases risk.
d. Smoking
- Smoking is a significant risk factor, particularly in individuals with a genetic predisposition.
e. Obesity
- Excess weight puts additional stress on the joints and increases inflammation.
f. Environmental Exposures
- Exposure to asbestos or silica may increase the risk of RA.
Diagnosis of Rheumatoid Arthritis
Early diagnosis is crucial for effective management of RA. The diagnostic process typically includes:
1. Medical History and Physical Examination
A doctor will begin by evaluating the patient’s symptoms, risk factors, and medical history.
A. Key Questions Asked
- When did joint pain and stiffness begin?
- Are the symptoms symmetrical (affecting both sides of the body)?
- Do symptoms improve with movement or worsen with rest?
- Any family history of autoimmune diseases?
- Presence of fatigue, fever, or weight loss?
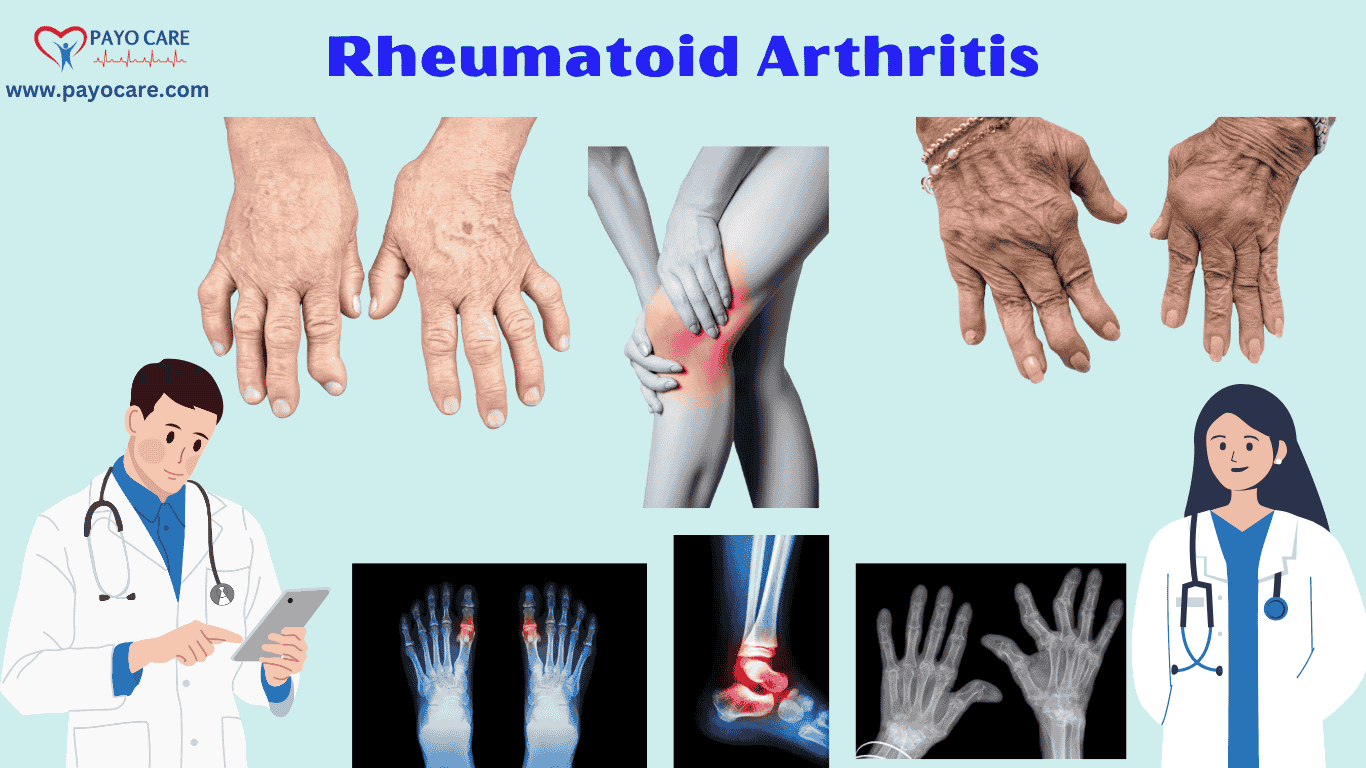
B. Physical Examination
The doctor will check for:
- Swelling, redness, and tenderness in joints
- Joint warmth and range of motion
- Rheumatoid nodules (firm lumps under the skin)
- Deformities in advanced cases
2. Laboratory Tests
A. Blood Tests
-
Rheumatoid Factor (RF) Test
- Detects antibodies associated with RA.
- Positive in ~70-80% of RA cases, but can be seen in other diseases.
-
Anti-Cyclic Citrullinated Peptide (Anti-CCP) Antibody Test
- More specific for RA than RF.
- Positive in ~60-70% of RA cases.
-
Erythrocyte Sedimentation Rate (ESR)
- Measures inflammation levels in the body.
- Higher ESR suggests active inflammation.
-
C-Reactive Protein (CRP) Test
- Detects inflammation and disease activity.
- High levels indicate active RA.
-
Complete Blood Count (CBC)
- Checks for anemia, which is common in RA patients.
3. Imaging Tests
A. X-rays
- Detects joint erosion, narrowing of joint spaces, and deformities in later stages.
B. Ultrasound
- Assesses synovial inflammation and early joint damage.
C. Magnetic Resonance Imaging (MRI)
- Provides detailed images of soft tissue and early-stage joint damage.
4. Classification Criteria for RA (ACR/EULAR 2010 Criteria)
Doctors use a scoring system (0-10 points) to confirm RA diagnosis. A score of ≥6 points suggests definite RA. The criteria include:
- Joint Involvement: Number and size of joints affected
- Serology: RF and anti-CCP antibody tests
- Acute Phase Reactants: ESR and CRP levels
- Duration of Symptoms: More than 6 weeks
5. Differential Diagnosis
RA symptoms may resemble:
- Osteoarthritis (OA) (degenerative joint disease)
- Lupus (SLE) (another autoimmune disorder)
- Psoriatic Arthritis
- Gout (caused by uric acid crystals)
- Infectious Arthritis

Treatment of Rheumatoid Arthritis
While there is no cure for RA, treatment aims to reduce inflammation, relieve symptoms, prevent joint damage, and improve quality of life.
a. Medications
- Disease-Modifying Antirheumatic Drugs (DMARDs): Methotrexate is the most commonly used DMARD.
- Biologic Agents: TNF inhibitors (e.g., etanercept) and other biologics target specific parts of the immune system.
- Corticosteroids: Used for short-term relief of severe symptoms.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Provide pain relief and reduce inflammation.
b. Lifestyle Modifications
- Exercise: Regular physical activity to maintain joint function and muscle strength.
- Diet: Anti-inflammatory foods and supplements like omega-3 fatty acids.
- Stress Management: Techniques like meditation or counseling to cope with chronic pain.
c. Physical Therapy
- Customized exercise programs to improve joint mobility and reduce pain.
d. Surgery
- Joint Replacement: For severely damaged joints, such as hip or knee replacement.
- Synovectomy: Removal of the inflamed synovium to reduce pain and swelling.
8. When to See a Doctor
Early intervention is key to managing RA effectively. Seek medical attention if you experience:
- Persistent joint pain, swelling, or stiffness, especially in the morning.
- Symptoms that interfere with daily activities.
- Systemic symptoms like fatigue, fever, or weight loss.
- A family history of RA or other autoimmune diseases.
Key Points
- What is rheumatoid arthritis?
- Rheumatoid arthritis symptoms
- Causes of rheumatoid arthritis
- Types of rheumatoid arthritis
- How to prevent rheumatoid arthritis
- Rheumatoid arthritis vs osteoarthritis
- Best treatment for rheumatoid arthritis
- Early signs of rheumatoid arthritis
- Diagnosis of rheumatoid arthritis
- Medications for rheumatoid arthritis
- Natural remedies for rheumatoid arthritis
- Can rheumatoid arthritis be cured?
- Foods to avoid with rheumatoid arthritis
- Exercise for rheumatoid arthritis
- Rheumatoid arthritis and fatigue
- Juvenile rheumatoid arthritis symptoms
- Rheumatoid arthritis complications
- How does rheumatoid arthritis affect the body?
- Best diet for rheumatoid arthritis
- Latest research on rheumatoid arthritis
10 FAQs on Rheumatoid Arthritis
1. What is rheumatoid arthritis?
Rheumatoid arthritis (RA) is a chronic autoimmune disease where the immune system mistakenly attacks the joints, causing inflammation, pain, and potential joint damage.
2. What causes rheumatoid arthritis?
The exact cause is unknown, but genetic factors, environmental triggers (like smoking or infections), and hormonal imbalances may contribute to its development.
3. What are the early symptoms of rheumatoid arthritis?
Early symptoms include joint pain, stiffness (especially in the morning), swelling, fatigue, low-grade fever, and loss of joint function.
4. How is rheumatoid arthritis diagnosed?
RA is diagnosed through physical examination, blood tests (Rheumatoid Factor, Anti-CCP, CRP, ESR), X-rays, and MRI scans to check for joint damage.
5. Can rheumatoid arthritis be cured?
There is no cure for RA, but treatments like medications, lifestyle changes, and physical therapy can help manage symptoms and slow progression.
6. What are the best treatments for rheumatoid arthritis?
Treatment includes nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, disease-modifying anti-rheumatic drugs (DMARDs), biologics, and in severe cases, surgery.
7. What foods should be avoided with rheumatoid arthritis?
Avoid processed foods, red meat, sugary drinks, fried foods, and dairy if it triggers inflammation. Anti-inflammatory foods like fish, nuts, and leafy greens may help.
8. How does exercise help with rheumatoid arthritis?
Low-impact exercises like swimming, yoga, and walking improve joint flexibility, reduce stiffness, and strengthen muscles to support the joints.
9. Can rheumatoid arthritis affect other parts of the body?
Yes, RA can affect the heart, lungs, eyes, skin, and blood vessels, leading to complications like cardiovascular disease and lung inflammation.
10. When should I see a doctor for rheumatoid arthritis?
See a doctor if you experience persistent joint pain, swelling, stiffness lasting more than 30 minutes in the morning, or unexplained fatigue and weight loss.
Conclusion
Rheumatoid arthritis is a complex and chronic condition that requires a multidisciplinary approach to management. By understanding its types, causes, symptoms, and treatment options, individuals can take proactive steps to manage their condition and improve their quality of life. Early diagnosis and treatment are crucial to preventing joint damage and complications. If you suspect you may have RA, consult a healthcare professional for a thorough evaluation and personalized treatment plan.