Sjögren’s syndrome is a chronic autoimmune disorder characterized by the immune system attacking the body’s moisture-producing glands, particularly the salivary and lacrimal glands. This results in symptoms such as dry eyes and dry mouth, which are the hallmark features of the condition. Sjögren’s syndrome can also affect other parts of the body, including the joints, skin, lungs, kidneys, and nervous system, leading to a wide range of systemic symptoms.
The condition can occur alone (primary Sjögren’s syndrome) or in conjunction with other autoimmune diseases (secondary Sjögren’s syndrome), such as rheumatoid arthritis or lupus. Sjögren’s syndrome is more common in women than in men, and it typically develops in individuals between the ages of 40 and 60.
This comprehensive guide will explore the various types of Sjögren’s syndrome, their causes, symptoms, prevention strategies, diagnostic methods, and treatment options. By understanding these aspects, individuals can better manage their condition and seek appropriate medical care when necessary.

Types of Sjögren’s Syndrome
Sjögren’s syndrome can be classified into two main types based on its presentation and association with other autoimmune diseases:
1. Primary Sjögren’s Syndrome
- Description: Primary Sjögren’s syndrome occurs independently of other autoimmune diseases. It is characterized by the immune system attacking the moisture-producing glands, leading to dry eyes and dry mouth.
- Symptoms: In addition to dry eyes and dry mouth, primary Sjögren’s syndrome can cause systemic symptoms, such as fatigue, joint pain, and organ involvement (e.g., lungs, kidneys, nervous system).
2. Secondary Sjögren’s Syndrome
- Description: Secondary Sjögren’s syndrome occurs in conjunction with other autoimmune diseases, such as rheumatoid arthritis, lupus, or scleroderma. The symptoms of Sjögren’s syndrome are present alongside the symptoms of the associated autoimmune disease.
- Symptoms: The symptoms of secondary Sjögren’s syndrome are similar to those of primary Sjögren’s syndrome, including dry eyes, dry mouth, and systemic involvement. However, the presence of another autoimmune disease may complicate the clinical picture.
Causes of Sjögren’s Syndrome
The exact cause of Sjögren’s syndrome is not fully understood, but it is believed to result from a combination of genetic, environmental, and immunological factors. The main causes and contributing factors include:
1. Genetic Predisposition
- Role of Genetics: Certain genetic factors may increase the risk of developing Sjögren’s syndrome. Individuals with a family history of autoimmune diseases are at higher risk.
- HLA Genes: Specific human leukocyte antigen (HLA) genes have been associated with an increased risk of Sjögren’s syndrome.
2. Autoimmune Response
- Mechanism: In Sjögren’s syndrome, the immune system mistakenly attacks the body’s moisture-producing glands, leading to inflammation and damage. This autoimmune response is thought to be triggered by a combination of genetic and environmental factors.
- Autoantibodies: The presence of autoantibodies, such as anti-SSA (Ro) and anti-SSB (La), is common in individuals with Sjögren’s syndrome and contributes to the autoimmune attack.
3. Environmental Triggers
- Infections: Certain viral or bacterial infections may trigger the onset of Sjögren’s syndrome in genetically predisposed individuals. Examples include Epstein-Barr virus (EBV) and hepatitis C virus (HCV).
- Hormonal Factors: Hormonal changes, particularly in women, may play a role in the development of Sjögren’s syndrome. The condition is more common in women, suggesting a potential link to estrogen and other hormones.
4. Immune System Dysregulation
- Cytokines: Dysregulation of cytokines, which are signaling molecules involved in the immune response, may contribute to the inflammation and tissue damage seen in Sjögren’s syndrome.
- B-Cell Activation: Abnormal activation of B-cells, a type of immune cell, is thought to play a role in the autoimmune response and the production of autoantibodies.
Symptoms of Sjögren’s Syndrome
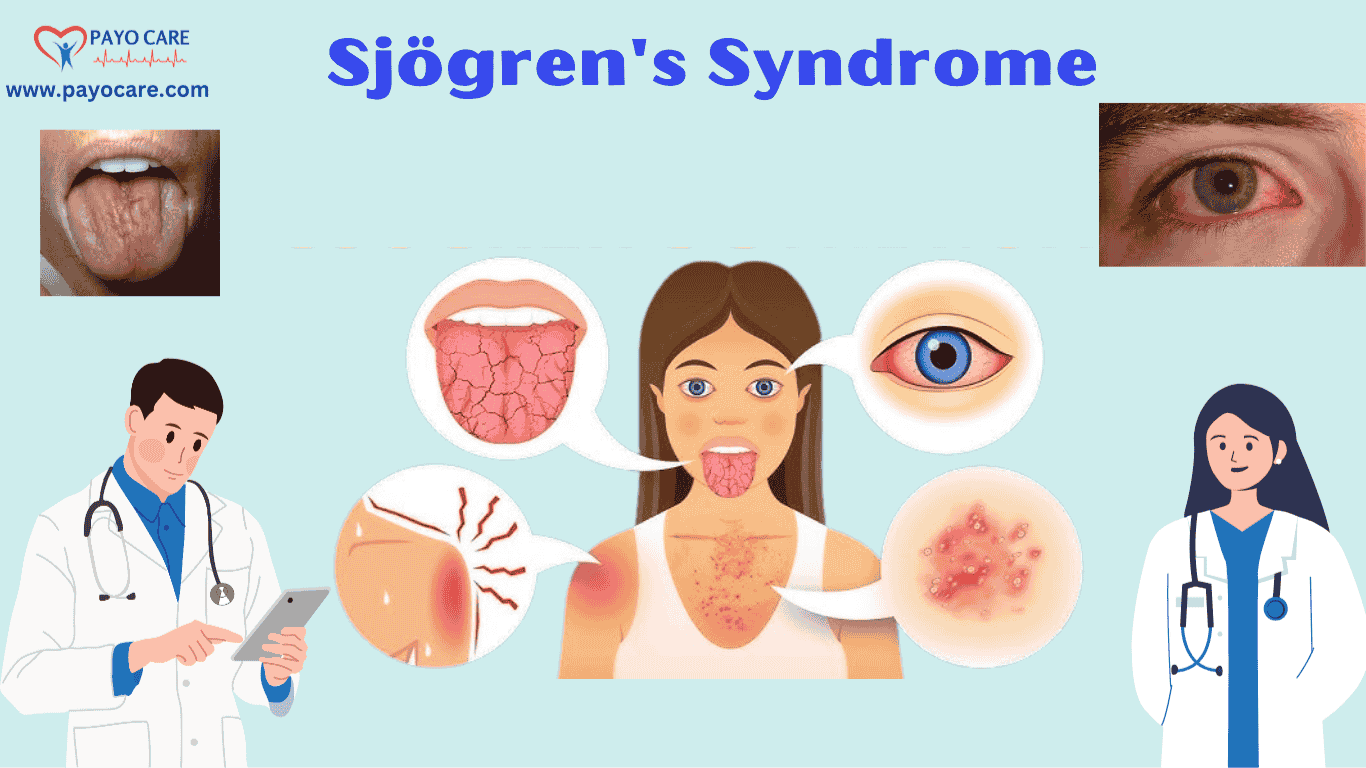
The symptoms of Sjögren’s syndrome can vary widely depending on the severity of the condition and the extent of glandular and systemic involvement. Common symptoms include:
1. Dry Eyes (Keratoconjunctivitis Sicca)
- Description: Dry eyes are a hallmark symptom of Sjögren’s syndrome, resulting from reduced tear production by the lacrimal glands.
- Symptoms: Individuals may experience a gritty or burning sensation in the eyes, redness, sensitivity to light, and blurred vision.
2. Dry Mouth (Xerostomia)
- Description: Dry mouth is another hallmark symptom, resulting from reduced saliva production by the salivary glands.
- Symptoms: Individuals may experience difficulty swallowing, speaking, and tasting, as well as an increased risk of dental cavities and oral infections.
3. Fatigue
- Description: Fatigue is a common systemic symptom of Sjögren’s syndrome and can be debilitating.
- Impact: Fatigue can significantly impact daily activities and quality of life.
4. Joint Pain and Stiffness
- Description: Joint pain and stiffness, similar to that seen in rheumatoid arthritis, can occur in individuals with Sjögren’s syndrome.
- Location: The pain and stiffness are often felt in the hands, wrists, and knees.
5. Swollen Salivary Glands
- Description: Swelling of the salivary glands, particularly the parotid glands, can occur in Sjögren’s syndrome.
- Symptoms: The swelling may be painful and can lead to a feeling of fullness or discomfort in the face.
6. Dry Skin and Mucous Membranes
- Description: Reduced moisture production can lead to dry skin and mucous membranes.
- Symptoms: Individuals may experience dry, itchy skin, as well as dryness in the nose, throat, and vagina.
7. Systemic Symptoms
- Description: Sjögren’s syndrome can affect various organs and systems, leading to a wide range of systemic symptoms.
- Examples: Systemic symptoms may include lung involvement (e.g., interstitial lung disease), kidney involvement (e.g., renal tubular acidosis), and nervous system involvement (e.g., peripheral neuropathy).
8. Dental and Oral Complications
- Description: Reduced saliva production can lead to dental and oral complications.
- Examples: Individuals may experience an increased risk of dental cavities, gum disease, and oral infections (e.g., oral thrush).
9. Raynaud’s Phenomenon
- Description: Raynaud’s phenomenon, characterized by cold-induced color changes in the fingers and toes, can occur in individuals with Sjögren’s syndrome.
- Symptoms: The fingers and toes may turn white, blue, and then red in response to cold or stress.

Prevention of Sjögren’s Syndrome
Since the exact cause of Sjögren’s syndrome is not fully understood, there are no specific prevention strategies. However, individuals can take steps to manage their symptoms and reduce the risk of complications:
1. Maintain Good Oral Hygiene
- Brushing and Flossing: Regular brushing and flossing can help prevent dental cavities and gum disease, which are common complications of dry mouth.
- Saliva Substitutes: Using saliva substitutes or sugar-free gum can help stimulate saliva production and alleviate dry mouth.
2. Eye Care
- Artificial Tears: Using artificial tears or lubricating eye drops can help alleviate dry eyes and prevent complications such as corneal ulcers.
- Humidifiers: Using a humidifier in the home can help maintain moisture in the air and reduce dryness in the eyes and mucous membranes.
3. Stay Hydrated
- Fluid Intake: Drinking plenty of water throughout the day can help alleviate dry mouth and maintain overall hydration.
- Avoid Caffeine and Alcohol: Limiting caffeine and alcohol intake can help prevent dehydration and reduce dryness.
4. Protect Against Infections
- Hand Hygiene: Practicing good hand hygiene can help reduce the risk of infections, particularly in individuals with dry mucous membranes.
- Vaccinations: Staying up-to-date with vaccinations, such as the flu vaccine and pneumococcal vaccine, can help prevent infections.
5. Manage Stress
- Stress-Reduction Techniques: Incorporating stress-reduction techniques, such as yoga, meditation, and deep breathing exercises, can help manage stress and reduce the risk of symptom flare-ups.
6. Regular Medical Check-Ups
- Monitoring: Regular check-ups with a healthcare provider can help monitor for early signs of complications and ensure that symptoms are well-managed.
Diagnosis of Sjögren’s Syndrome
The diagnosis of Sjögren’s syndrome involves a combination of clinical evaluation, laboratory tests, and diagnostic procedures. The goal is to assess the extent of glandular and systemic involvement and rule out other conditions with similar symptoms. The diagnostic process typically includes the following steps:
1. Medical History and Physical Examination
- Patient History: The healthcare provider will take a detailed medical history, including any symptoms, family history of autoimmune diseases, and exposure to environmental triggers.
- Physical Examination: A thorough physical examination will be performed to assess for signs of dryness, glandular swelling, and systemic involvement.
2. Schirmer’s Test
- Procedure: The Schirmer’s test measures tear production by placing a small strip of filter paper under the lower eyelid for five minutes.
- Interpretation: Reduced tear production (less than 5 mm of wetting) is indicative of dry eyes and may suggest Sjögren’s syndrome.
3. Salivary Gland Function Tests
- Salivary Flow Rate: The salivary flow rate test measures the amount of saliva produced over a specific period. Reduced saliva production may indicate Sjögren’s syndrome.
- Sialography: Sialography involves injecting a contrast dye into the salivary glands and taking X-rays to assess glandular function and structure.
4. Blood Tests
- Autoantibodies: Blood tests may be performed to detect the presence of autoantibodies, such as anti-SSA (Ro) and anti-SSB (La), which are commonly associated with Sjögren’s syndrome.
- Inflammatory Markers: Elevated levels of inflammatory markers, such as erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), may indicate inflammation.
5. Lip Biopsy
- Procedure: A lip biopsy involves removing a small sample of salivary gland tissue from the lower lip for microscopic examination.
- Interpretation: The presence of lymphocytic infiltration (immune cells) in the salivary glands is a hallmark feature of Sjögren’s syndrome.
6. Imaging Studies
- Ultrasound: Ultrasound imaging of the salivary glands can help assess glandular structure and detect abnormalities.
- MRI or CT Scan: In some cases, MRI or CT scans may be used to evaluate glandular and systemic involvement.
7. Ocular Staining
- Procedure: Ocular staining involves applying a dye to the surface of the eye to assess for damage to the cornea and conjunctiva.
- Interpretation: The presence of corneal or conjunctival staining is indicative of dry eyes and may suggest Sjögren’s syndrome.

Treatment of Sjögren’s Syndrome
The treatment of Sjögren’s syndrome focuses on managing symptoms, preventing complications, and addressing systemic involvement. Treatment options range from lifestyle modifications and medications to more invasive procedures in severe cases. The main treatment approaches include:
1. Lifestyle Modifications
- Eye Care: Using artificial tears, lubricating eye drops, and humidifiers can help alleviate dry eyes and prevent complications.
- Oral Hygiene: Maintaining good oral hygiene, using saliva substitutes, and staying hydrated can help manage dry mouth and prevent dental complications.
- Dietary Changes: Eating a balanced diet rich in vitamins and minerals can support overall health and reduce the risk of complications.
2. Medications
- Artificial Tears and Lubricants: Over-the-counter artificial tears and lubricating eye drops can help alleviate dry eyes.
- Saliva Stimulants: Medications such as pilocarpine (Salagen) and cevimeline (Evoxac) can help stimulate saliva production and alleviate dry mouth.
- Anti-Inflammatory Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) can help reduce joint pain and inflammation.
- Immunosuppressive Medications: In cases of severe systemic involvement, immunosuppressive medications, such as corticosteroids or methotrexate, may be prescribed to reduce inflammation and immune system activity.
3. Dental Care
- Regular Check-Ups: Regular dental check-ups and cleanings are essential for preventing dental cavities and gum disease.
- Fluoride Treatments: Using fluoride toothpaste and receiving fluoride treatments can help strengthen tooth enamel and prevent cavities.
4. Systemic Treatments
- Hydroxychloroquine: Hydroxychloroquine (Plaquenil) is an antimalarial medication that can help reduce systemic symptoms, such as joint pain and fatigue.
- Biologic Therapies: Biologic therapies, such as rituximab (Rituxan), may be used in severe cases to target specific components of the immune system and reduce inflammation.
5. Surgical Interventions
- Punctal Plugs: Punctal plugs can be inserted into the tear ducts to block drainage and retain moisture in the eyes, alleviating dry eyes.
- Salivary Gland Surgery: In rare cases, surgical intervention may be necessary to address complications related to salivary gland swelling or dysfunction.
6. Alternative and Complementary Therapies
- Acupuncture: Acupuncture may help alleviate symptoms such as dry mouth and dry eyes by stimulating specific points on the body.
- Herbal Remedies: Some individuals may explore herbal remedies, such as evening primrose oil or flaxseed oil, to alleviate symptoms. However, the efficacy and safety of these remedies are not well-established, and they should be used with caution.
7. Psychological Support
- Counseling: Living with a chronic autoimmune condition can be challenging, and counseling or therapy can help individuals cope with the emotional and psychological impact of Sjögren’s syndrome.
- Support Groups: Joining a support group can provide a sense of community and shared experiences, helping individuals feel less isolated.
Conclusion
Sjögren’s syndrome is a chronic autoimmune disorder that primarily affects the moisture-producing glands, leading to symptoms such as dry eyes and dry mouth. The condition can also have systemic effects, impacting various organs and systems. While the exact cause of Sjögren’s syndrome is not fully understood, it is believed to result from a combination of genetic, environmental, and immunological factors.
Prevention of Sjögren’s syndrome involves managing symptoms, maintaining good oral and eye hygiene, and seeking regular medical care. Early diagnosis and appropriate treatment are crucial for managing the condition and preventing potential complications, such as dental cavities, corneal ulcers, and systemic involvement.
By understanding the types, causes, symptoms, prevention strategies, diagnostic methods, and treatment options for Sjögren’s syndrome, individuals can take proactive steps to manage their condition and improve their quality of life. With the right approach, it is possible to effectively manage Sjögren’s syndrome and maintain overall health and well-being.
1. What is Sjögren’s Syndrome?
Sjögren’s Syndrome is an autoimmune disorder where the immune system attacks the body’s moisture-producing glands, primarily affecting the eyes and mouth.
2. What are the types of Sjögren’s Syndrome?
There are two types:
- Primary Sjögren’s Syndrome – Occurs independently without another autoimmune disease.
- Secondary Sjögren’s Syndrome – Develops alongside another autoimmune condition, such as rheumatoid arthritis or lupus.
3. What causes Sjögren’s Syndrome?
The exact cause is unknown, but it is believed to result from a combination of genetic, environmental, and immune system factors.
4. What are the common symptoms of Sjögren’s Syndrome?
Symptoms include:
- Dry eyes and dry mouth
- Difficulty swallowing
- Joint pain and swelling
- Fatigue
- Dry skin
- Swollen salivary glands
5. Who is at risk for Sjögren’s Syndrome?
It primarily affects women over 40, but it can occur at any age. Individuals with a family history of autoimmune diseases have a higher risk.
6. Can Sjögren’s Syndrome be prevented?
There is no known way to prevent Sjögren’s Syndrome, but managing risk factors like reducing stress, avoiding smoking, and maintaining good hydration can help alleviate symptoms.
7. How is Sjögren’s Syndrome diagnosed?
Diagnosis involves:
- Blood tests (checking for autoantibodies)
- Schirmer’s test (measuring tear production)
- Salivary gland biopsy
- Eye examinations
8. What are the complications of Sjögren’s Syndrome?
Complications include:
- Increased risk of dental cavities
- Vision problems due to chronic dry eyes
- Lung, liver, and kidney issues
- Higher risk of lymphoma (a type of cancer)
9. How is Sjögren’s Syndrome treated?
Treatment focuses on symptom management, including:
- Artificial tears and saliva substitutes
- Anti-inflammatory medications
- Immunosuppressive drugs
- Lifestyle changes, such as staying hydrated
10. Is there a cure for Sjögren’s Syndrome?
No, there is no cure, but treatments help manage symptoms and improve the quality of life.