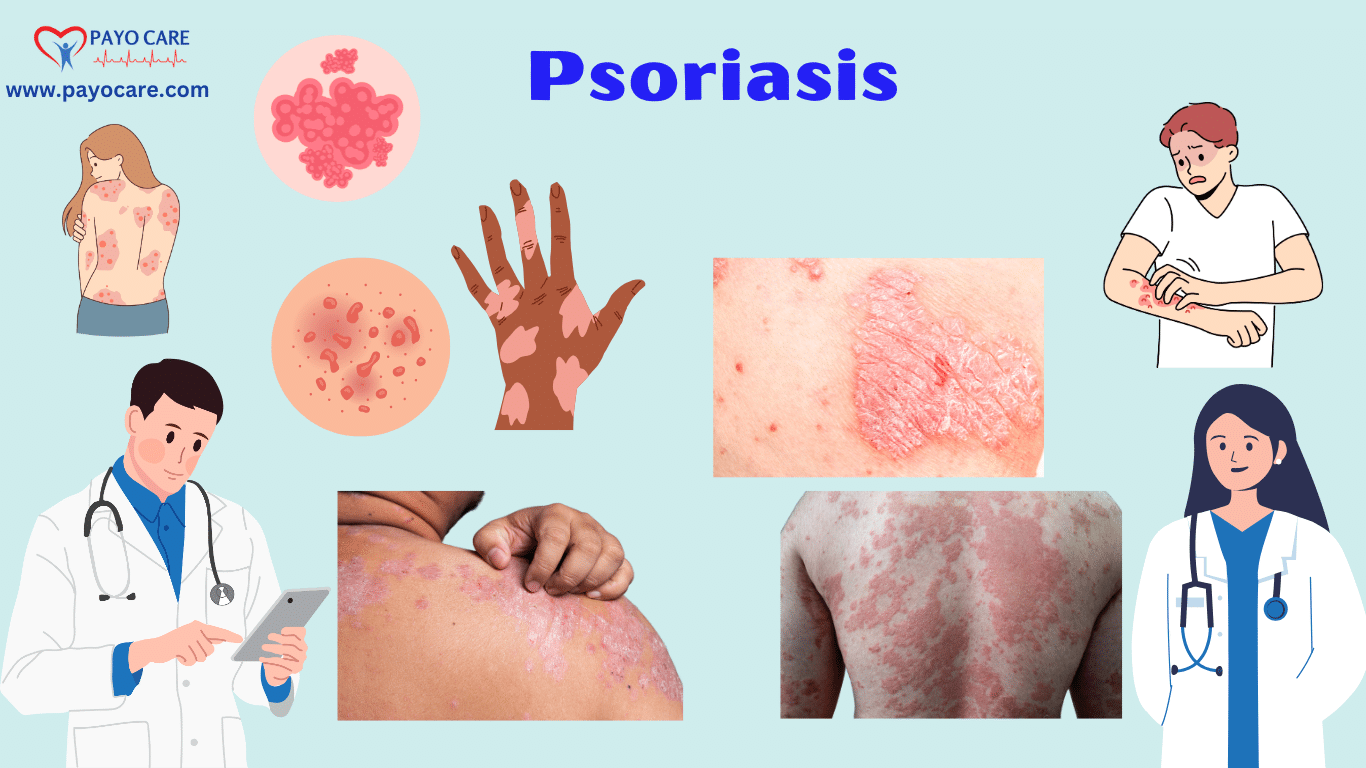
Psoriasis is a long-term autoimmune condition that causes skin cells to grow too quickly. This leads to a buildup of cells on the skin’s surface, resulting in scaling, redness, and inflammation. While not contagious, psoriasis can greatly affect a person’s daily life, impacting their physical and emotional well-being. Learning about its causes, symptoms, types, prevention, and treatment can help manage the condition better.
Types of Psoriasis
There are several types of psoriasis, each with distinct characteristics:
- Plaque Psoriasis: The most common type, causing raised, red patches covered with silvery scales. It often appears on the scalp, elbows, knees, and lower back. These patches can be itchy and sometimes painful, leading to discomfort in daily activities.
- Guttate Psoriasis: Small, drop-like sores, usually triggered by infections like strep throat. It is more common in children and young adults, often appearing suddenly and covering large areas of the body.
- Inverse Psoriasis: Smooth, red, and shiny lesions appearing in skin folds such as under the breasts, around the groin, and under the arms. The condition can be aggravated by sweating and friction.
- Pustular Psoriasis: White pustules filled with pus on red, inflamed skin, often affecting the hands and feet. This type can be painful and may come with flu-like symptoms, including fever and chills.
- Erythrodermic Psoriasis: The most severe type, leading to widespread redness, severe peeling, and pain. It requires immediate medical attention as it can lead to serious complications like infection and dehydration.
Causes of Psoriasis
The exact cause of psoriasis is not fully understood. However, it is linked to an overactive immune system that speeds up skin cell growth. Instead of shedding naturally, new skin cells build up, forming scaly patches. Genetic factors also play a role, as psoriasis tends to run in families. External triggers that can worsen the condition include:
- Stress: High levels of stress can weaken the immune system, triggering flare-ups.
- Infections: Bacterial and viral infections can cause immune system disruptions that lead to psoriasis symptoms.
- Skin injuries: Cuts, burns, bug bites, and sunburns can lead to new patches of psoriasis.
- Medications: Some drugs, such as beta-blockers, lithium, and anti-malarial medications, can exacerbate psoriasis.
- Smoking and Alcohol: Both have been linked to an increased risk of developing psoriasis and worsening symptoms.
Symptoms of Psoriasis
Symptoms vary based on the type and severity of psoriasis. Common signs include:
- Red patches of skin covered with thick, silvery scales
- Itching, burning, or soreness, which can range from mild to severe
- Cracked and dry skin that may bleed
- Nail changes like pitting, discoloration, or separation from the nail bed
- Joint pain, stiffness, and swelling, which are signs of psoriatic arthritis
Since psoriasis is a chronic condition, it can also affect mental health, leading to stress, anxiety, and depression. The visible nature of the disease can impact self-esteem and social interactions.

Preventing Psoriasis Flare-Ups
While psoriasis cannot be prevented entirely, certain measures can help reduce flare-ups:
- Manage Stress: Practicing relaxation techniques like yoga, meditation, and breathing exercises can help control stress levels.
- Avoid Triggers: Identifying and avoiding triggers like infections, smoking, and alcohol can help manage the condition.
- Moisturize Regularly: Keeping skin well-moisturized prevents dryness and cracking, reducing irritation.
- Follow a Healthy Diet: A diet rich in anti-inflammatory foods, such as leafy greens, fatty fish, and nuts, can help reduce inflammation.
- Exercise Regularly: Maintaining a healthy weight helps reduce the severity of symptoms, especially for those with psoriatic arthritis.
Diagnosing Psoriasis
A dermatologist usually diagnoses psoriasis by examining the skin, nails, and scalp. In some cases, a skin biopsy may be done to confirm the condition. If joint pain is present, imaging tests like X-rays or MRIs may help diagnose psoriatic arthritis. Blood tests are not typically used for psoriasis but may be done to rule out other conditions.
Treatment Options for Psoriasis
The treatment of psoriasis depends on its severity. Common options include:
- Topical Treatments:
- Corticosteroids: Reduce inflammation and itching.
- Vitamin D Analogs: Slow down skin cell growth.
- Moisturizers: Prevent dryness and cracking.
- Phototherapy:
- Controlled exposure to ultraviolet (UV) light slows down excessive skin cell growth and reduces symptoms.
- Systemic Medications:
- Biologics: Target specific immune system pathways and have shown excellent results in controlling psoriasis symptoms.
- Methotrexate: Slows cell growth and suppresses inflammation.
- Cyclosporine: Suppresses the immune system and reduces flare-ups.
- Oral Retinoids: Help control severe cases but may cause side effects like dry skin and liver issues.
Frequently Asked Questions (FAQs)
1. Is psoriasis contagious?
No, psoriasis is not contagious. It is an autoimmune condition and cannot be spread from person to person.
2. Can psoriasis be cured?
There is no cure for psoriasis, but treatments help manage symptoms effectively.
3. What triggers psoriasis flare-ups?
Common triggers include stress, infections, skin injuries, medications, smoking, and alcohol.
4. Can diet affect psoriasis?
A healthy diet rich in anti-inflammatory foods can help manage symptoms.
5. Does psoriasis affect only the skin?
No, psoriasis can also affect nails and joints, leading to psoriatic arthritis.
6. What is the best treatment for psoriasis?
Treatment varies depending on severity. Topical treatments, phototherapy, and systemic medications are common options.
7. Can stress worsen psoriasis?
Yes, stress is a known trigger for psoriasis flare-ups.
8. Is psoriasis hereditary?
Yes, genetics play a significant role, and it often runs in families.
Conclusion
Psoriasis is a lifelong condition, but the right treatment and lifestyle adjustments can help manage symptoms. Seeking professional medical advice and following prescribed treatments can improve quality of life and prevent complications. Taking proactive steps, such as managing stress, maintaining a healthy lifestyle, and avoiding triggers, can help keep symptoms under control. If you suspect you have psoriasis, consulting a dermatologist is essential for an accurate diagnosis and personalized treatment plan.