Cardiomyopathy is a severe disease of the heart muscle that affects its ability to pump blood efficiently. It can lead to complications such as heart failure, arrhythmias, and even sudden cardiac arrest. The condition can be inherited or acquired due to various lifestyle and medical factors. Understanding the different types of cardiomyopathy, their causes, symptoms, and treatment options is crucial for effective management and prevention.
Types of Cardiomyopathy
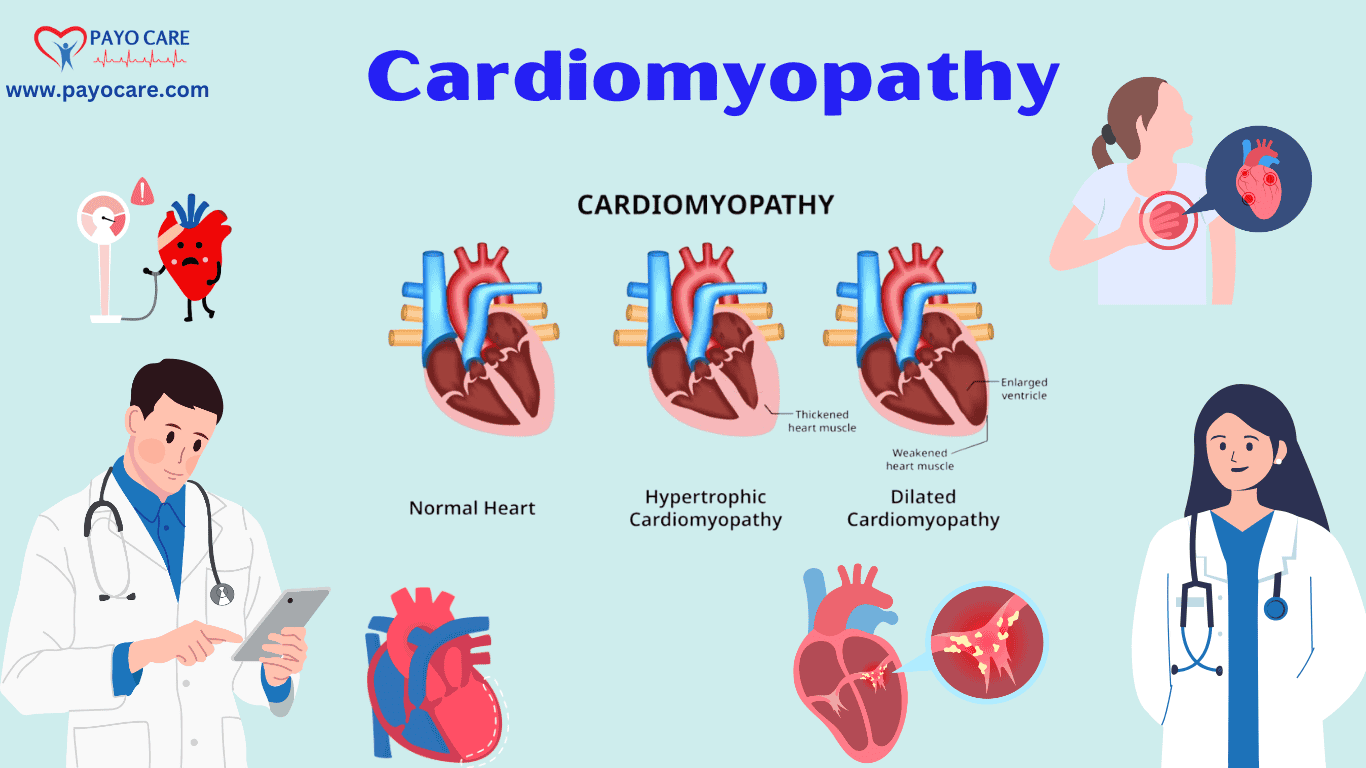
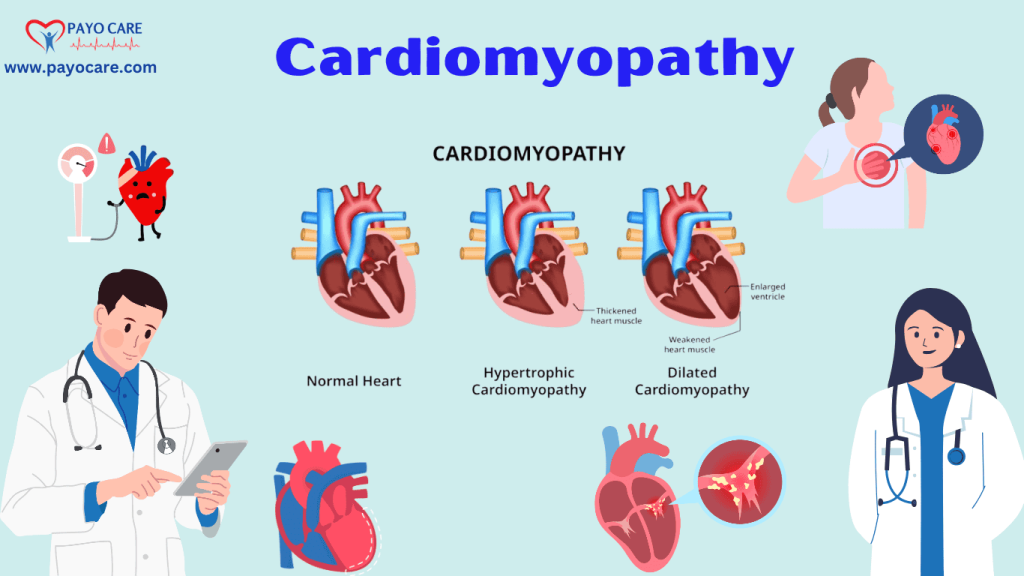
Cardiomyopathy is broadly classified into several types, each affecting the heart muscle differently. The main types include:
1. Dilated Cardiomyopathy (DCM)
Dilated cardiomyopathy is the most common form, where the heart’s main pumping chamber (left ventricle) becomes enlarged and weakened, reducing its efficiency in pumping blood.
Causes:
- Genetic factors
- Viral infections (e.g., myocarditis)
- Alcohol abuse
- High blood pressure
- Chemotherapy drugs
- Thyroid disorders
Symptoms:
- Shortness of breath
- Fatigue
- Swelling in the legs and feet
- Irregular heartbeats
- Dizziness
2. Hypertrophic Cardiomyopathy (HCM)
Hypertrophic cardiomyopathy is characterized by an abnormal thickening of the heart muscle, particularly the left ventricle, which obstructs blood flow.
Causes:
- Genetic mutations
- High blood pressure
- Aging-related changes
Symptoms:
- Chest pain
- Shortness of breath
- Lightheadedness
- Fainting during physical activity
3. Restrictive Cardiomyopathy (RCM)
Restrictive cardiomyopathy is a rare condition where the heart muscle becomes rigid, losing its ability to expand and fill with blood properly.
Causes:
- Amyloidosis (abnormal protein deposits in the heart)
- Hemochromatosis (excess iron accumulation)
- Radiation therapy or chemotherapy
Symptoms:
- Fatigue
- Swelling in the legs
- Shortness of breath
- Abnormal heart rhythms
4. Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC)
ARVC is a rare, inherited disorder that primarily affects the right ventricle, replacing heart muscle with fatty or fibrous tissue, leading to arrhythmias.
Causes:
- Genetic mutations
- Family history of heart disorders
Symptoms:
- Palpitations
- Dizziness
- Fainting
- Sudden cardiac arrest in severe cases
5. Takotsubo Cardiomyopathy (Stress-Induced)
Also known as “broken heart syndrome,” this condition is triggered by extreme emotional or physical stress and results in temporary weakening of the left ventricle.
Causes:
- Severe emotional distress (e.g., grief, shock)
- Physical stressors (e.g., sudden illness, surgery)
Symptoms:
- Chest pain
- Shortness of breath
- Irregular heartbeats
- Fainting
Causes and Risk Factors
Cardiomyopathy may be caused by various factors, including:
1. Genetic Factors
Many forms of cardiomyopathy are hereditary, meaning they run in families. Genetic mutations can lead to abnormal heart muscle development.
2. Lifestyle and Environmental Factors
- Alcohol and drug abuse
- Poor diet and obesity
- High blood pressure
- Sedentary lifestyle
3. Underlying Medical Conditions
- Diabetes
- Autoimmune diseases
- Chronic kidney disease
- Thyroid disorders
4. Viral and Bacterial Infections
Certain infections can cause inflammation of the heart muscle (myocarditis), leading to cardiomyopathy.
5. Medications and Toxins
Some drugs, including chemotherapy medications, corticosteroids, and excessive alcohol use, can weaken the heart muscle over time.
Symptoms of Cardiomyopathy
Symptoms vary depending on the type and severity but commonly include:
- Shortness of breath, even at rest
- Swelling in the lower extremities (edema)
- Fatigue and weakness
- Palpitations or irregular heartbeats
- Dizziness, fainting, or chest pain
- Reduced exercise tolerance
Prevention of Cardiomyopathy
While some types of cardiomyopathy are genetic and unavoidable, lifestyle modifications can help reduce the risk.
1. Maintain a Healthy Diet
A balanced diet rich in fruits, vegetables, whole grains, and lean proteins promotes heart health.
2. Regular Exercise
Engaging in moderate physical activity strengthens the heart and improves circulation.
3. Control Blood Pressure and Cholesterol
Managing hypertension and cholesterol levels through diet, exercise, and medications reduces heart strain.
4. Avoid Excessive Alcohol and Drug Use
Limiting alcohol intake and avoiding illicit drugs help prevent heart damage.
5. Manage Stress
Practicing relaxation techniques such as meditation, deep breathing, or yoga can prevent stress-induced cardiomyopathy.
6. Routine Medical Checkups
Regular doctor visits can help detect early signs of cardiomyopathy and manage risk factors.
Diagnosis of Cardiomyopathy
A comprehensive diagnosis involves a combination of medical history, physical examination, and specialized tests.
1. Medical History and Physical Examination
A doctor will review symptoms, family history, and potential risk factors contributing to cardiomyopathy.
2. Diagnostic Tests
- Echocardiogram: Uses ultrasound to assess heart structure and function.
- Electrocardiogram (ECG): Records electrical activity and detects arrhythmias.
- Cardiac MRI: Provides detailed images of the heart muscle.
- Chest X-ray: Identifies heart enlargement.
- Blood Tests: Detects markers of heart disease or infections.
- Cardiac Catheterization: Measures pressure inside the heart chambers and evaluates function.
- Stress Test: Assesses heart performance during exercise.
Treatment Options for Cardiomyopathy
Treatment depends on the type and severity of the condition and may include medications, lifestyle changes, medical devices, or surgery.
1. Medications
- Beta-blockers: Reduce heart rate and lower blood pressure.
- ACE Inhibitors: Relax blood vessels to improve circulation.
- Diuretics: Reduce fluid buildup and alleviate swelling.
- Antiarrhythmic Drugs: Help manage abnormal heart rhythms.
- Blood Thinners: Prevent clot formation and stroke.
2. Lifestyle Changes
- Low-sodium diet
- Regular physical activity
- Smoking cessation
- Stress management
3. Medical Devices
- Pacemakers: Regulate heartbeats in arrhythmia patients.
- Implantable Cardioverter Defibrillator (ICD): Prevents sudden cardiac death.
- Cardiac Resynchronization Therapy (CRT): Enhances heart function in advanced cases.
4. Surgical and Advanced Treatments
- Septal Myectomy: Removes thickened heart muscle in HCM patients.
- Heart Transplant: Reserved for severe cases where other treatments fail.
- Left Ventricular Assist Device (LVAD): A mechanical pump used for end-stage heart failure patients.
Key points
- Cardiomyopathy disease
- Heart muscle disorder
- Weak heart pumping
- Types of cardiomyopathy
- Cardiomyopathy causes & symptoms
- Heart disease diagnosis
- Cardiomyopathy treatment options
- Lifestyle changes for heart health
Cardiomyopathy: 10 Frequently Asked Questions (FAQs)
1. What is Cardiomyopathy?
Cardiomyopathy is a disease that affects the heart muscle, making it harder for the heart to pump blood to the rest of the body. It can lead to heart failure and other complications if not managed properly.
2. What are the different types of Cardiomyopathy?
The main types of cardiomyopathy include:
- Dilated Cardiomyopathy (DCM): The heart chambers enlarge and weaken.
- Hypertrophic Cardiomyopathy (HCM): The heart muscle thickens abnormally.
- Restrictive Cardiomyopathy (RCM): The heart muscle becomes stiff, restricting blood flow.
- Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC): Fatty and fibrous tissue replaces heart muscle, causing irregular rhythms.
- Takotsubo Cardiomyopathy: A temporary heart condition caused by extreme stress.
3. What causes Cardiomyopathy?
Common causes include:
- Genetic factors (family history)
- High blood pressure
- Heart attacks and coronary artery disease
- Viral infections affecting the heart
- Excessive alcohol or drug use
- Autoimmune diseases
- Metabolic disorders (such as diabetes)
4. What are the symptoms of Cardiomyopathy?
Symptoms vary but commonly include:
- Shortness of breath
- Fatigue and weakness
- Swelling in legs, ankles, and feet
- Irregular heartbeats (arrhythmias)
- Chest pain or discomfort
- Dizziness or fainting
5. How is Cardiomyopathy diagnosed?
Doctors use several tests to diagnose cardiomyopathy, such as:
- Electrocardiogram (ECG): Checks heart rhythms.
- Echocardiogram: Uses ultrasound to examine heart structure.
- Cardiac MRI: Provides detailed heart imaging.
- Chest X-ray: Detects heart enlargement.
- Stress Test: Evaluates heart performance under exertion.
- Genetic Testing: Identifies hereditary risks.
6. Can Cardiomyopathy be prevented?
While some forms are genetic and unavoidable, you can lower the risk by:
- Maintaining a heart-healthy diet
- Exercising regularly
- Avoiding alcohol and smoking
- Managing stress
- Controlling underlying conditions like high blood pressure and diabetes
7. What are the treatment options for Cardiomyopathy?
Treatment depends on the type and severity of the disease and may include:
- Medications: Beta-blockers, ACE inhibitors, diuretics, and blood thinners
- Lifestyle changes: Healthy diet, exercise, and stress management
- Medical devices: Pacemakers and implantable defibrillators (ICDs)
- Surgery: Heart transplants or procedures like septal myectomy for severe cases
8. Is Cardiomyopathy a life-threatening condition?
It can be life-threatening if left untreated, as it may lead to heart failure, arrhythmias, or sudden cardiac arrest. However, early diagnosis and proper treatment can help manage the condition.
9. Can Cardiomyopathy be inherited?
Yes, certain types, such as hypertrophic cardiomyopathy and arrhythmogenic right ventricular cardiomyopathy, have a genetic basis and can be passed down in families.
10. When should I see a doctor for Cardiomyopathy?
Seek medical attention if you experience:
- Persistent shortness of breath
- Unexplained fatigue or dizziness
- Irregular or rapid heartbeats
- Chest pain or discomfort
- Swelling in the legs and feet
Conclusion
Cardiomyopathy is a complex and potentially life-threatening condition that requires careful diagnosis and management. By understanding the types, causes, symptoms, prevention strategies, diagnostic methods, and treatment options, individuals can take proactive steps to manage their condition and improve their quality of life. Early diagnosis and a comprehensive treatment plan are crucial for reducing the risk of complications and enhancing outcomes. With proper care, including lifestyle modifications, medications, and advanced therapies, individuals with cardiomyopathy can lead healthier, more fulfilling lives. Ongoing research and awareness are essential for advancing our understanding of cardiomyopathy and developing more effective prevention and treatment strategies.