Hemophilia is a rare genetic bleeding disorder that impairs the body’s ability to form blood clots, leading to prolonged bleeding after injuries or surgeries. It primarily affects males, though females can be carriers of the condition. Hemophilia can range from mild to severe, depending on the level of clotting factors in the blood. In this comprehensive guide, we’ll explore the types, causes, symptoms, prevention, diagnosis, and treatment of hemophilia to help you better understand this condition.
What is Hemophilia?
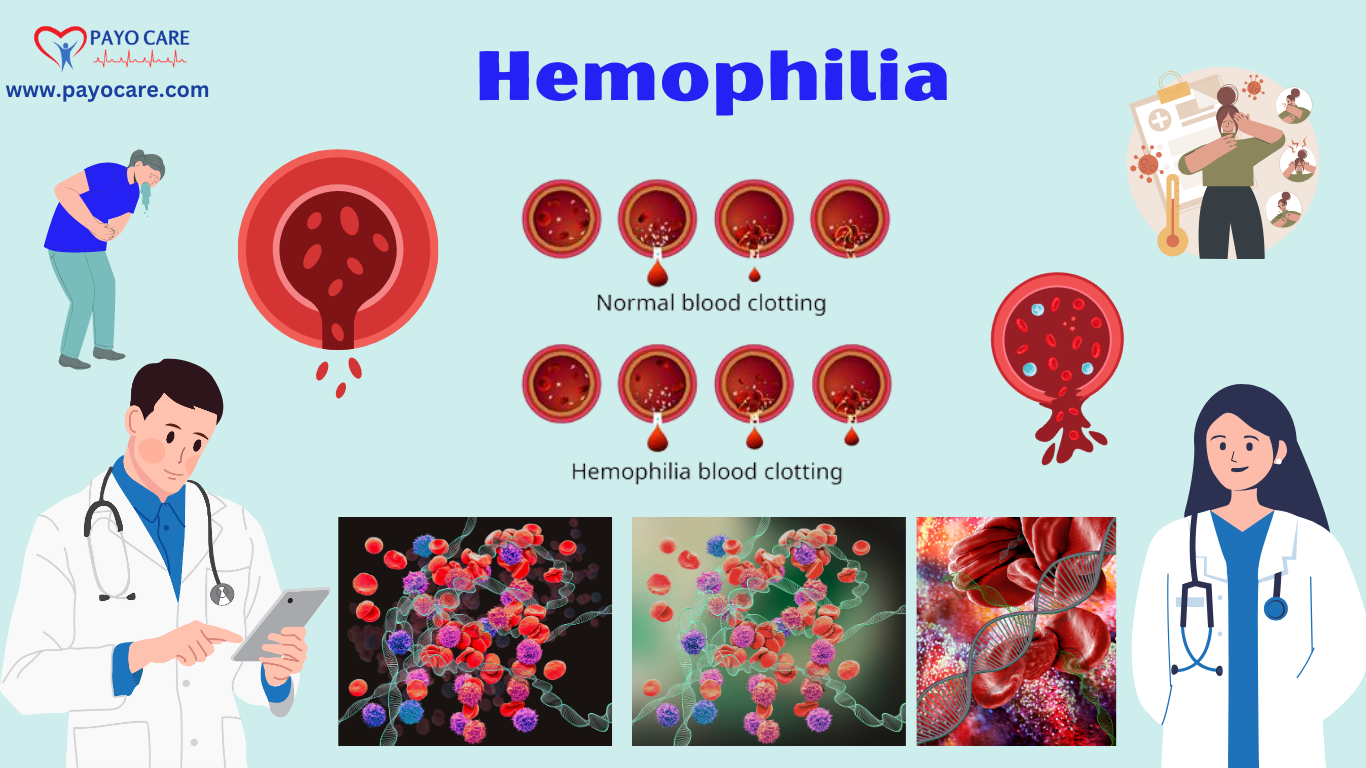
Hemophilia is a hereditary bleeding disorder caused by a deficiency or absence of specific clotting factors in the blood. These clotting factors are proteins that help the blood clot and stop bleeding. Without sufficient clotting factors, even minor injuries can result in excessive bleeding, and internal bleeding can occur spontaneously, particularly in the joints and muscles.
Types of Hemophilia
There are two main types of hemophilia, classified based on the deficient clotting factor:
1. Hemophilia A (Classic Hemophilia)
- Caused by a deficiency of clotting factor VIII.
- Most common type, affecting about 80% of people with hemophilia.
2. Hemophilia B (Christmas Disease)
- Caused by a deficiency of clotting factor IX.
- Less common than Hemophilia A.
3. Hemophilia C
- Caused by a deficiency of clotting factor XI.
- Rare and typically milder than Hemophilia A and B.
Causes of Hemophilia
Hemophilia is primarily caused by genetic mutations that affect the production of clotting factors. Key causes include:
- Inherited Genetic Mutation:
- Hemophilia is an X-linked recessive disorder, meaning the gene mutation is located on the X chromosome.
- Males (XY) are more likely to develop hemophilia because they have only one X chromosome.
- Females (XX) are usually carriers and may pass the gene to their children.
- Spontaneous Mutation:
- In about one-third of cases, hemophilia occurs due to a spontaneous mutation with no family history.
- Acquired Hemophilia:
- Rarely, hemophilia can develop later in life due to autoimmune disorders, cancer, or pregnancy.
Symptoms of Hemophilia
The symptoms of hemophilia depend on the severity of the condition. Common signs include:
- Prolonged Bleeding: After injuries, surgeries, or dental procedures.
- Frequent Nosebleeds: Without an obvious cause.
- Easy Bruising: Large or deep bruises from minor bumps.
- Joint Bleeding (Hemarthrosis): Swelling, pain, and stiffness in joints like knees, elbows, and ankles.
- Muscle Bleeding: Pain, swelling, and tightness in muscles.
- Blood in Urine or Stool: Indicating internal bleeding.
- Excessive Bleeding After Vaccinations: Or minor cuts.
- Unexplained Irritability (in Infants): A sign of internal bleeding.
In severe cases, bleeding into the brain (intracranial hemorrhage) can occur, which is life-threatening.

Prevention of Hemophilia
Since hemophilia is a genetic disorder, it cannot be prevented. However, the following steps can help manage the condition and reduce complications:
- Genetic Counseling:
- Families with a history of hemophilia should seek genetic counseling before planning a pregnancy.
- Avoid High-Risk Activities:
- Avoid contact sports or activities with a high risk of injury.
- Regular Check-Ups:
- Monitor clotting factor levels and overall health.
- Vaccinations:
- Get vaccinated against hepatitis A and B to prevent liver-related complications.
- Bleeding Precautions:
- Use soft-bristled toothbrushes and avoid medications like aspirin that can increase bleeding.
Diagnosis of Hemophilia
If hemophilia is suspected, a healthcare provider will perform several tests to confirm the diagnosis:
- Family History:
- Assess the presence of hemophilia in family members.
- Blood Tests:
- Measure the levels of clotting factors VIII and IX.
- Check the time it takes for blood to clot (prothrombin time and activated partial thromboplastin time).
- Genetic Testing:
- Identify specific gene mutations responsible for hemophilia.
- Prenatal Testing:
- For families with a history of hemophilia, tests like amniocentesis or chorionic villus sampling can detect the condition in a fetus.
Treatment of Hemophilia
While there is no cure for hemophilia, effective treatments can help manage the condition and prevent complications. Treatment options include:
1. Replacement Therapy
- Regular infusions of clotting factor concentrates (factor VIII or IX) to prevent or stop bleeding.
- Can be administered prophylactically (preventively) or on-demand (after bleeding occurs).
2. Desmopressin (DDAVP)
- A synthetic hormone that stimulates the release of stored factor VIII in mild hemophilia A.
3. Gene Therapy
- An emerging treatment that aims to introduce a functional copy of the defective gene to produce clotting factors.
4. Antifibrinolytic Medications
- Help prevent the breakdown of blood clots.
- Examples: Tranexamic acid or aminocaproic acid.
5. Physical Therapy
- For individuals with joint damage due to repeated bleeding.
6. First Aid for Bleeding
- Apply pressure to the wound.
- Use ice packs to reduce swelling.
- Elevate the affected area.
7. Avoid Certain Medications:
- Avoid aspirin and nonsteroidal anti-inflammatory drugs (NSAIDs) that can increase bleeding risk.
Living with Hemophilia
Living with hemophilia requires careful management and lifestyle adjustments. Here are some tips:
- Stay Active: Engage in low-impact exercises like swimming or walking to strengthen muscles and joints.
- Maintain a Healthy Diet: Support overall health and maintain a healthy weight to reduce stress on joints.
- Educate Yourself: Learn about hemophilia and how to manage bleeding episodes.
- Carry Medical ID: Wear a medical alert bracelet or carry a card indicating your condition.
- Seek Support: Join support groups or connect with others living with hemophilia.
When to See a Doctor
Seek immediate medical attention if you experience:
- Severe or uncontrolled bleeding.
- Signs of internal bleeding (e.g., blood in urine or stool).
- Joint swelling, pain, or stiffness.
- Headache, vomiting, or confusion (possible signs of brain bleeding).
Conclusion
Hemophilia is a lifelong condition that requires careful management, but with proper treatment and precautions, individuals with hemophilia can lead healthy and active lives. Early diagnosis, regular medical care, and adherence to treatment plans are essential to prevent complications. By staying informed and taking proactive steps, you can effectively manage hemophilia and improve your quality of life.
Share this guide to raise awareness and support those affected by hemophilia.