Morphine is one of the most well-known and widely used opioid medications in the world. It has been a cornerstone in the management of pain for over a century, providing relief to millions of patients suffering from acute and chronic pain conditions. Despite its effectiveness, morphine is a potent drug with a high potential for abuse and addiction, making it a controlled substance in most countries. This article will provide a comprehensive overview of morphine, including its uses, benefits, side effects, dosage, and warnings.
What is Morphine?
Morphine is a natural opioid alkaloid derived from the opium poppy plant, Papaver somniferum. It was first isolated in 1804 by the German pharmacist Friedrich Sertürner, who named it after Morpheus, the Greek god of dreams, due to its sleep-inducing properties. Morphine is classified as an opioid agonist, meaning it binds to specific receptors in the brain and spinal cord to produce its effects.
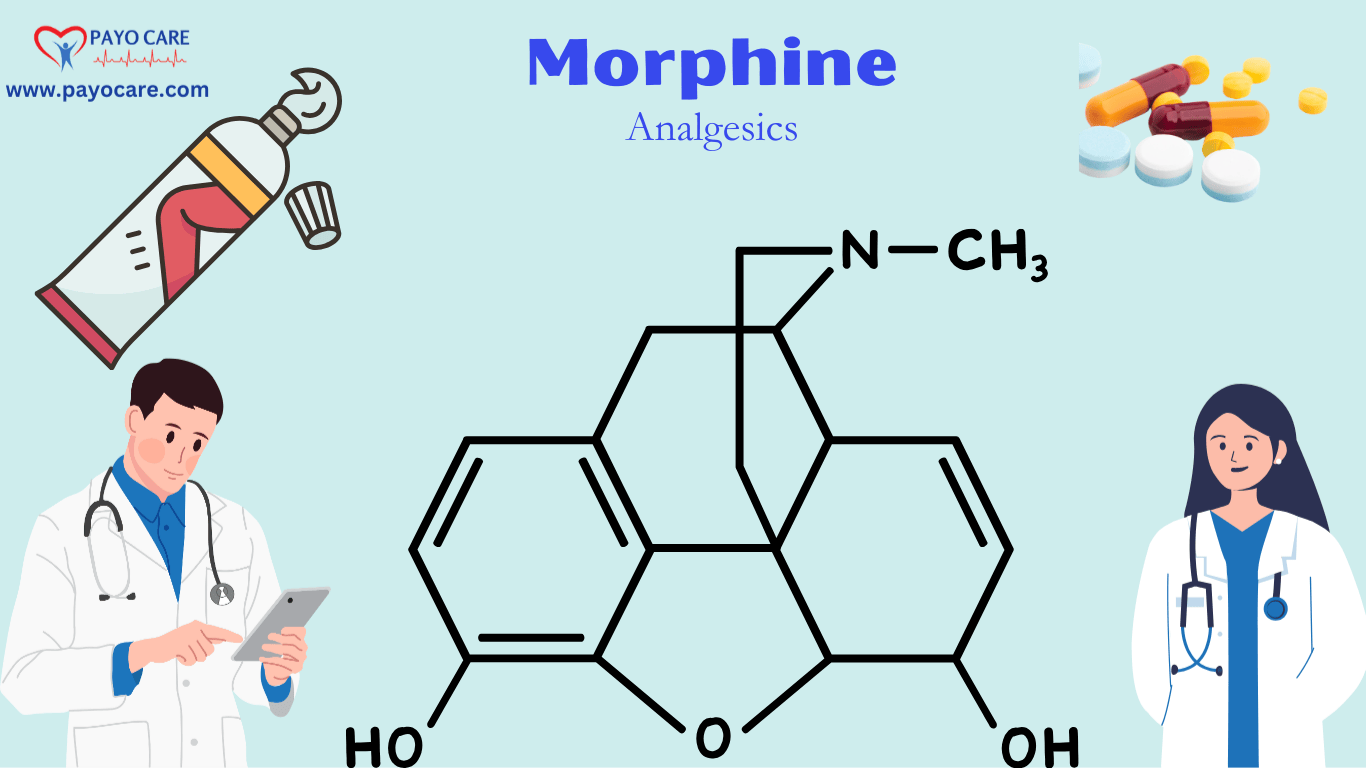
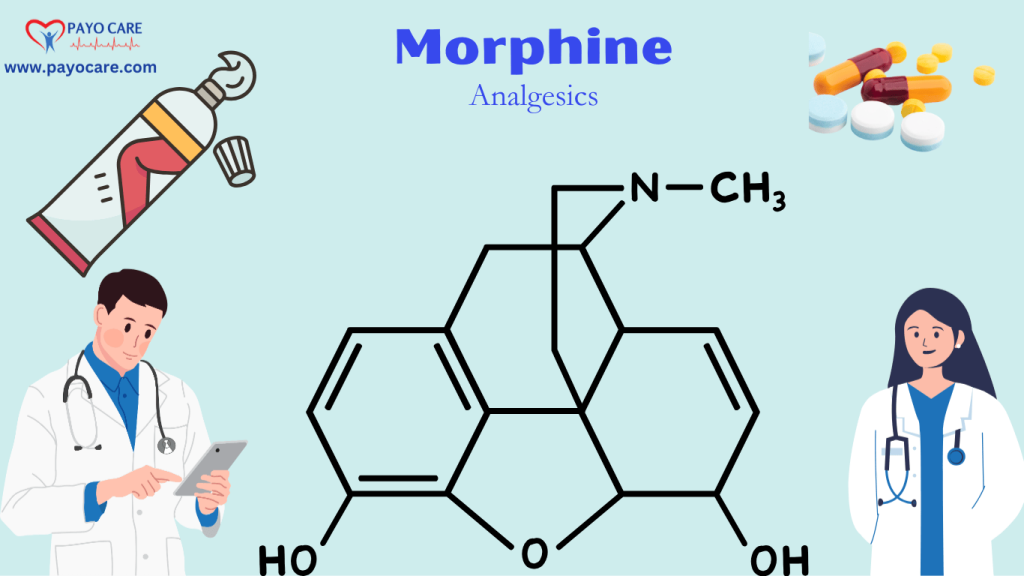
Chemical Structure and Mechanism of Action
Morphine’s chemical structure is characterized by a pentacyclic ring system, which is essential for its pharmacological activity. It primarily acts on the mu-opioid receptors (MOR) in the central nervous system (CNS), although it also has some affinity for kappa-opioid receptors (KOR) and delta-opioid receptors (DOR). By binding to these receptors, morphine inhibits the transmission of pain signals and alters the perception of pain, leading to analgesia (pain relief).
In addition to its analgesic effects, morphine also affects other systems in the body, including the respiratory, gastrointestinal, and cardiovascular systems. These effects are mediated through the activation of opioid receptors in various tissues and organs.
Uses of Morphine
Morphine is primarily used for the management of pain, but it has several other medical applications as well. Below are the main uses of morphine:
1. Pain Management
Morphine is most commonly prescribed for the relief of moderate to severe pain. It is particularly effective in managing pain associated with:
- Post-Surgical Pain: Morphine is often administered after major surgeries to control acute pain. It can be given intravenously (IV), intramuscularly (IM), or through patient-controlled analgesia (PCA) pumps.
- Cancer Pain: Morphine is a first-line treatment for cancer-related pain, especially in patients with advanced stages of the disease. It is often used in combination with other analgesics to provide adequate pain relief.
- Trauma Pain: In cases of severe trauma, such as fractures, burns, or crush injuries, morphine can be used to manage acute pain.
- Chronic Pain: While morphine is generally not the first choice for chronic non-cancer pain due to the risk of tolerance and dependence, it may be used in certain cases where other treatments have failed.
2. Palliative Care
In palliative care settings, morphine is used to alleviate pain and improve the quality of life for patients with terminal illnesses. It is often administered in the form of oral solutions, tablets, or patches to provide continuous pain relief.
3. Acute Myocardial Infarction (Heart Attack)
Morphine is sometimes used in the emergency treatment of acute myocardial infarction (heart attack) to relieve chest pain (angina) and reduce anxiety. However, its use in this context has become more controversial due to potential adverse effects on cardiovascular function.
4. Pulmonary Edema
Morphine can be used to treat acute pulmonary edema (fluid accumulation in the lungs) associated with left ventricular failure. It works by reducing preload and afterload on the heart, leading to decreased pulmonary congestion.
5. Anesthesia
Morphine is sometimes used as an adjunct to general anesthesia to provide intraoperative and postoperative analgesia. It can also be used in regional anesthesia techniques, such as epidural or intrathecal administration, to provide localized pain relief.
6. Cough Suppression
Although less common today, morphine has historically been used as a cough suppressant, particularly in cases of severe, intractable cough. However, due to its potential for abuse and the availability of safer alternatives, its use for this purpose has declined.
Benefits of Morphine
Morphine offers several benefits, particularly in the context of pain management and palliative care. Some of the key benefits include:
1. Effective Pain Relief
Morphine is one of the most potent analgesics available, making it highly effective for managing severe pain. Its ability to provide rapid and sustained pain relief is particularly valuable in acute settings, such as post-surgical care or trauma.
2. Versatility in Administration
Morphine can be administered through various routes, including oral, intravenous, intramuscular, subcutaneous, epidural, and intrathecal. This versatility allows healthcare providers to tailor the treatment to the patient’s specific needs and circumstances.
3. Improved Quality of Life
For patients with chronic or terminal illnesses, morphine can significantly improve quality of life by alleviating pain and reducing suffering. In palliative care, it allows patients to remain comfortable and maintain dignity during their final days.
4. Rapid Onset of Action
When administered intravenously, morphine has a rapid onset of action, typically within 5 to 10 minutes. This makes it particularly useful in emergency situations where quick pain relief is needed.
5. Cost-Effectiveness
Morphine is relatively inexpensive compared to some other opioid analgesics, making it accessible to a broader population. This is especially important in low-resource settings where cost is a significant factor in healthcare decision-making.
Side Effects of Morphine
While morphine is highly effective for pain relief, it is associated with a range of side effects, some of which can be serious. The side effects of morphine are primarily related to its action on opioid receptors in the CNS and other tissues. Below are the most common side effects:
1. Central Nervous System Effects
- Sedation and Drowsiness: Morphine can cause significant sedation, which may impair a patient’s ability to perform tasks that require alertness, such as driving or operating machinery.
- Euphoria: Some patients may experience a sense of euphoria or well-being, which contributes to the drug’s potential for abuse.
- Respiratory Depression: One of the most serious side effects of morphine is respiratory depression, which can lead to decreased breathing rate and, in severe cases, respiratory arrest. This is particularly concerning in patients with pre-existing respiratory conditions or those receiving high doses of the drug.
- Confusion and Cognitive Impairment: Morphine can cause confusion, disorientation, and impaired cognitive function, especially in elderly patients or those with underlying cognitive disorders.
- Dependence and Addiction: Long-term use of morphine can lead to physical dependence and addiction. Patients may develop tolerance, requiring higher doses to achieve the same level of pain relief, and may experience withdrawal symptoms if the drug is abruptly discontinued.
2. Gastrointestinal Effects
- Nausea and Vomiting: Morphine can stimulate the chemoreceptor trigger zone in the brain, leading to nausea and vomiting. This is more common when the drug is first started or when the dose is increased.
- Constipation: Morphine slows down gastrointestinal motility, leading to constipation. This is one of the most common and persistent side effects, often requiring the use of laxatives or stool softeners.
- Abdominal Cramping: Some patients may experience abdominal cramping or discomfort due to the effects of morphine on the gastrointestinal tract.
3. Cardiovascular Effects
- Hypotension: Morphine can cause a drop in blood pressure, particularly when administered intravenously. This is due to its vasodilatory effects and can be problematic in patients with pre-existing hypotension or cardiovascular disease.
- Bradycardia: Morphine may slow down the heart rate (bradycardia), which can be concerning in patients with certain heart conditions.
4. Other Side Effects
- Urinary Retention: Morphine can cause difficulty in urination or urinary retention, particularly in elderly men with prostate enlargement.
- Pruritus (Itching): Some patients may experience itching or a rash, which is thought to be related to the release of histamine.
- Miosis (Pupil Constriction): Morphine causes constriction of the pupils (miosis), which is a characteristic sign of opioid use.
- Sweating: Excessive sweating (diaphoresis) is another potential side effect of morphine.
Dosage and Administration
The dosage of morphine varies depending on the patient’s age, weight, medical condition, and the route of administration. It is crucial to individualize the dose to achieve adequate pain relief while minimizing side effects. Below are general guidelines for morphine dosage and administration:
1. Oral Administration
- Immediate-Release Tablets or Solutions: The typical starting dose for adults is 10 to 30 mg every 4 hours as needed for pain. For opioid-naive patients, a lower starting dose of 5 to 10 mg may be appropriate.
- Extended-Release Tablets or Capsules: These formulations are designed for around-the-clock pain management and are typically dosed every 8 to 12 hours. The starting dose is usually 15 to 30 mg every 12 hours, with adjustments made based on the patient’s response.
2. Intravenous (IV) Administration
- Bolus Dosing: For acute pain, the typical IV dose is 2.5 to 15 mg every 4 hours as needed. The dose should be titrated carefully to avoid respiratory depression.
- Continuous Infusion: In some cases, morphine may be administered as a continuous IV infusion, particularly in postoperative or critically ill patients. The infusion rate is typically started at 0.8 to 10 mg per hour and adjusted based on pain control and side effects.
3. Intramuscular (IM) or Subcutaneous (SC) Administration
- The typical IM or SC dose is 5 to 20 mg every 4 hours as needed for pain. This route is less commonly used today due to the availability of IV and oral formulations.
4. Epidural or Intrathecal Administration
- Epidural: The typical epidural dose is 1 to 5 mg, with a maximum of 10 mg per 24 hours. This route is often used for postoperative pain management.
- Intrathecal: The intrathecal dose is much lower, typically 0.1 to 0.3 mg, due to the direct delivery of the drug to the spinal cord.
5. Pediatric Dosage
- The dosage for children is typically based on weight, with a starting dose of 0.1 to 0.2 mg/kg every 4 hours as needed. Careful monitoring is essential to avoid overdose and respiratory depression.
6. Geriatric Dosage
- Elderly patients may require lower doses due to decreased metabolism and increased sensitivity to opioids. A starting dose of 2.5 to 5 mg every 4 hours is often recommended.
7. Renal or Hepatic Impairment
- Patients with renal or hepatic impairment may require dose adjustments or longer dosing intervals to avoid accumulation of the drug and increased risk of side effects.

Warnings and Precautions
Morphine is a powerful medication with a high potential for abuse, addiction, and serious side effects. Therefore, it should be used with caution and under close medical supervision. Below are some important warnings and precautions associated with morphine use:
1. Risk of Respiratory Depression
Morphine can cause life-threatening respiratory depression, particularly in patients who are opioid-naive, elderly, or have pre-existing respiratory conditions. Careful monitoring of respiratory rate and oxygen saturation is essential, especially during the initial dosing period and after dose increases.
2. Risk of Addiction and Dependence
Morphine has a high potential for abuse and addiction, even when used as prescribed. Patients with a history of substance abuse or mental health disorders are at increased risk. Long-term use should be avoided unless absolutely necessary, and patients should be regularly assessed for signs of dependence or addiction.
3. Risk of Overdose
Morphine overdose can be fatal, particularly when the drug is taken in large doses or combined with other CNS depressants, such as alcohol, benzodiazepines, or other opioids. Symptoms of overdose include severe respiratory depression, extreme drowsiness, cold and clammy skin, and loss of consciousness. Naloxone, an opioid antagonist, is the treatment of choice for morphine overdose.
4. Use in Pregnancy and Lactation
Morphine should be used with caution during pregnancy, as it can cross the placenta and affect the developing fetus. Prolonged use during pregnancy can lead to neonatal opioid withdrawal syndrome (NOWS) in the newborn. Morphine is also excreted in breast milk and can cause sedation and respiratory depression in nursing infants.
5. Use in Elderly Patients
Elderly patients are more sensitive to the effects of morphine and are at increased risk of side effects, such as respiratory depression, sedation, and cognitive impairment. Lower doses and careful monitoring are recommended in this population.
6. Use in Patients with Renal or Hepatic Impairment
Patients with renal or hepatic impairment may have reduced clearance of morphine, leading to increased drug levels and a higher risk of side effects. Dose adjustments and close monitoring are necessary in these patients.
7. Interactions with Other Medications
Morphine can interact with other medications, particularly CNS depressants, such as benzodiazepines, sedatives, and alcohol. These interactions can increase the risk of respiratory depression, sedation, and overdose. Patients should be advised to avoid alcohol and other CNS depressants while taking morphine.
8. Withdrawal Symptoms
Abrupt discontinuation of morphine after long-term use can lead to withdrawal symptoms, such as anxiety, agitation, sweating, nausea, vomiting, and muscle aches. To prevent withdrawal, the dose should be tapered gradually under medical supervision.
9. Tolerance
With prolonged use, patients may develop tolerance to morphine, requiring higher doses to achieve the same level of pain relief. This can increase the risk of side effects and overdose. Regular reassessment of the patient’s pain management plan is essential to minimize the risk of tolerance.
10. Driving and Operating Machinery
Morphine can cause drowsiness, sedation, and impaired cognitive function, which can affect a patient’s ability to drive or operate machinery. Patients should be advised to avoid these activities until they know how morphine affects them.
Conclusion
Morphine is a powerful and effective opioid analgesic that has been used for over a century to manage pain. Its ability to provide rapid and sustained pain relief makes it invaluable in various medical settings, including post-surgical care, cancer pain management, and palliative care. However, morphine is also associated with a range of side effects, including respiratory depression, sedation, constipation, and the potential for addiction and dependence.
The use of morphine requires careful consideration of the patient’s medical history, pain condition, and risk factors for side effects. It should be prescribed at the lowest effective dose for the shortest duration necessary to manage pain. Patients should be closely monitored for signs of respiratory depression, addiction, and other adverse effects.
In conclusion, while morphine is a highly effective medication for pain relief, it must be used with caution and under close medical supervision to minimize the risks associated with its use. Healthcare providers should educate patients about the potential side effects and risks of morphine and work with them to develop a safe and effective pain management plan.
1. What is Morphine used for?
Morphine is a strong opioid pain reliever used to treat moderate to severe pain, such as pain from surgery, injury, cancer, or chronic conditions. It works by blocking pain signals in the brain and nervous system.
2. What are the benefits of Morphine?
Morphine provides powerful pain relief, improves quality of life for patients with severe pain, and is often used in palliative care for those with terminal illnesses.
3. What are the common side effects of Morphine?
Common side effects include drowsiness, dizziness, nausea, vomiting, constipation, dry mouth, and sweating. These effects may decrease as your body adjusts to the medication.
4. Can Morphine cause addiction?
Yes, Morphine has a high potential for addiction, dependence, and misuse. Long-term use can lead to tolerance, meaning higher doses may be needed for the same effect. It should be taken exactly as prescribed.
5. How should Morphine be taken?
Morphine should be taken exactly as prescribed by a doctor. It is available in tablet, capsule, liquid, and injectable forms. Extended-release tablets should never be crushed or chewed.
6. What should I do if I miss a dose of Morphine?
If you miss a dose, take it as soon as you remember. If it’s almost time for your next dose, skip the missed one and continue with your regular schedule. Do not double the dose.
7. Who should avoid taking Morphine?
People with severe asthma, breathing problems, head injuries, liver or kidney disease, or a history of drug abuse should consult a doctor before using Morphine.
8. Can Morphine interact with other medications?
Yes, Morphine can interact with alcohol, sedatives, muscle relaxants, antidepressants, and other opioids, increasing the risk of dangerous side effects like respiratory depression.
9. What are the signs of a Morphine overdose?
Symptoms of overdose include slow or shallow breathing, extreme drowsiness, confusion, cold or clammy skin, and loss of consciousness. Seek emergency medical help if an overdose is suspected.
10. Can Morphine be used during pregnancy or breastfeeding?
Morphine is not recommended during pregnancy or breastfeeding, as it can cause withdrawal symptoms in newborns or pass into breast milk, affecting the baby. Always consult a doctor before use.