Pulmonary fibrosis is a chronic and progressive lung disease characterized by the scarring of lung tissue. This scarring, known as fibrosis, makes the lungs stiff and less efficient at transferring oxygen into the bloodstream. As a result, patients experience symptoms like shortness of breath, a persistent dry cough, and fatigue. While the exact cause of pulmonary fibrosis is often unknown, it can be triggered by environmental factors, genetic predisposition, or underlying health conditions. In this comprehensive guide, we’ll explore the types, causes, symptoms, prevention, diagnosis, and treatments of pulmonary fibrosis, providing you with the knowledge to manage this condition effectively.
What is Pulmonary Fibrosis?
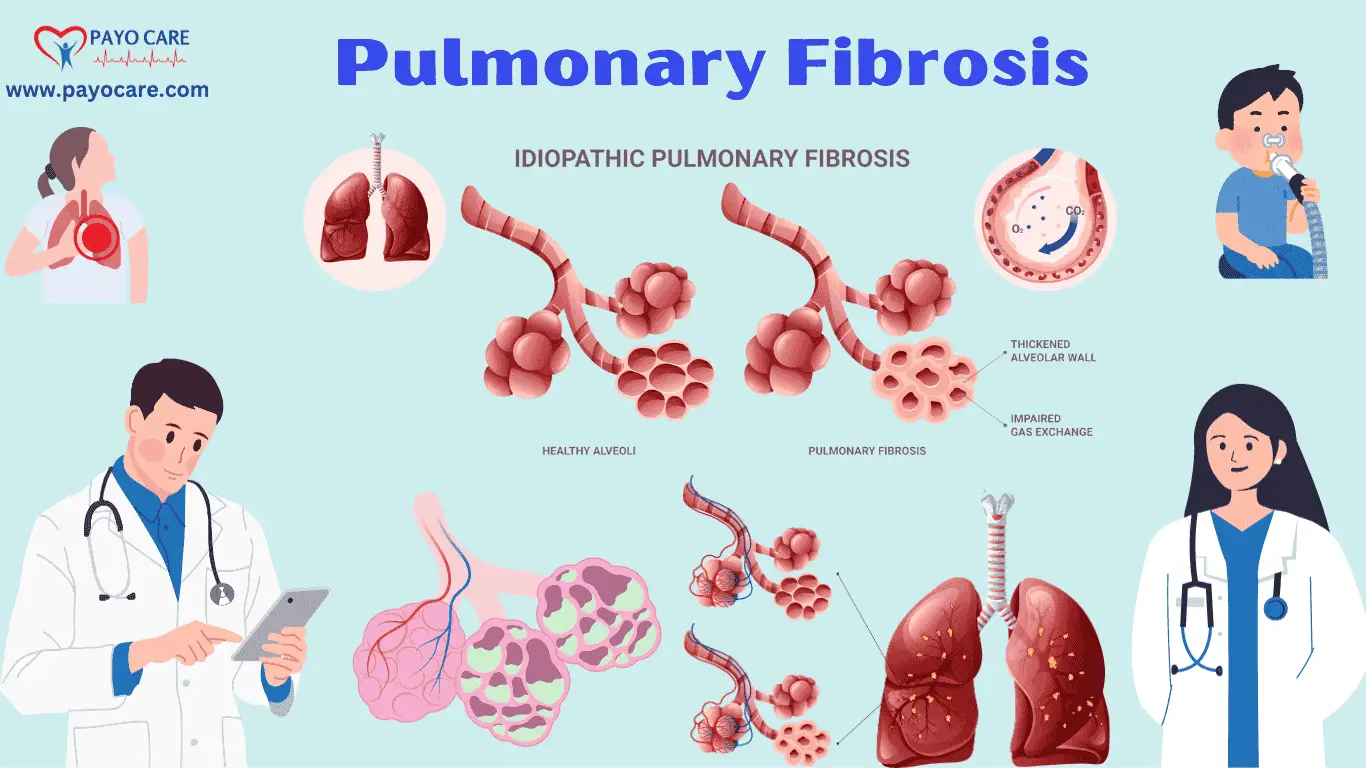
Pulmonary fibrosis occurs when the lung tissue becomes damaged and scarred, leading to reduced lung function. The scarring thickens and stiffens the tissue around the air sacs (alveoli), making it harder for oxygen to pass into the bloodstream. Over time, this can lead to respiratory failure and other complications. Pulmonary fibrosis can develop gradually or progress rapidly, depending on the type and cause. It is estimated that over 100,000 people in the United States are affected by idiopathic pulmonary fibrosis (IPF), the most common form of the disease.

Types of Pulmonary Fibrosis
There are several types of pulmonary fibrosis, classified based on their causes and underlying conditions:
1. Idiopathic Pulmonary Fibrosis (IPF)
Idiopathic pulmonary fibrosis is the most common form of pulmonary fibrosis, with no identifiable cause. It primarily affects adults over the age of 50 and is characterized by a progressive decline in lung function.
2. Occupational and Environmental Pulmonary Fibrosis
Exposure to certain environmental and occupational hazards can cause pulmonary fibrosis. Common causes include:
- Asbestosis (exposure to asbestos fibers)
- Silicosis (exposure to silica dust, often found in mining and construction)
- Coal Workers’ Pneumoconiosis (black lung disease from coal dust inhalation)
- Hypersensitivity Pneumonitis (chronic inhalation of mold, bacteria, or animal proteins)
3. Autoimmune-Related Pulmonary Fibrosis
Certain autoimmune diseases can lead to pulmonary fibrosis, including:
- Rheumatoid arthritis
- Systemic lupus erythematosus (SLE)
- Scleroderma
- Sjögren’s syndrome
- Polymyositis/dermatomyositis
4. Drug-Induced Pulmonary Fibrosis
Some medications and medical treatments can damage lung tissue and contribute to fibrosis. These include:
- Chemotherapy drugs (e.g., bleomycin, methotrexate)
- Radiation therapy (damage from radiation exposure to the lungs)
- Certain antibiotics (e.g., nitrofurantoin)
- Heart medications (e.g., amiodarone)
5. Genetic Pulmonary Fibrosis
Some cases of pulmonary fibrosis run in families, indicating a genetic predisposition to the disease. Mutations in specific genes (such as TERT and TERC) are associated with familial pulmonary fibrosis.
Causes of Pulmonary Fibrosis
Pulmonary fibrosis can be caused by multiple factors, including:
- Long-term exposure to environmental toxins (dust, chemicals, and pollutants)
- Infections (viral and bacterial infections can cause lung inflammation)
- Autoimmune diseases (immune system attacks lung tissue)
- Radiation therapy (lung damage from cancer treatment)
- Genetic predisposition (family history of pulmonary fibrosis)
- Unknown causes (idiopathic pulmonary fibrosis)
Symptoms of Pulmonary Fibrosis
Symptoms of pulmonary fibrosis vary based on disease severity and progression. Common symptoms include:
- Persistent dry cough
- Shortness of breath (dyspnea), especially during physical activity
- Fatigue and weakness
- Unexplained weight loss
- Chest discomfort or pain
- Clubbing of the fingers (thickening of the fingertips)
- Cyanosis (bluish discoloration of lips and nails due to low oxygen levels)
Prevention of Pulmonary Fibrosis
Although not all cases of pulmonary fibrosis can be prevented, certain measures can reduce the risk of developing the disease:
- Avoid exposure to lung irritants (smoke, pollutants, chemicals, and dust)
- Wear protective gear in workplaces with hazardous airborne particles
- Quit smoking and avoid secondhand smoke
- Get vaccinated against infections such as influenza and pneumonia
- Seek early treatment for autoimmune and lung diseases
- Maintain a healthy lifestyle with regular exercise and a balanced diet
Diagnosis of Pulmonary Fibrosis
Diagnosing pulmonary fibrosis requires a combination of clinical evaluation, imaging, and laboratory tests:
1. Medical History and Physical Examination
A doctor will assess symptoms, family history, and occupational exposure to lung irritants.
2. Imaging Tests
- High-Resolution CT (HRCT) Scan: Provides detailed images of lung scarring.
- Chest X-ray: Helps detect lung abnormalities but is less precise than HRCT.
3. Pulmonary Function Tests (PFTs)
- Measures lung capacity and airflow restriction.
4. Oxygen Level Measurement
- Pulse oximetry and arterial blood gas tests determine oxygen levels in the blood.
5. Bronchoscopy and Lung Biopsy
- Invasive tests to examine lung tissue for further analysis.

Treatment of Pulmonary Fibrosis
While there is no cure, treatments help manage symptoms and slow disease progression.
1. Medications
- Antifibrotic drugs (e.g., pirfenidone, nintedanib) slow lung scarring.
- Anti-inflammatory drugs may be used in autoimmune-related fibrosis.
- Oxygen therapy helps maintain blood oxygen levels.
2. Pulmonary Rehabilitation
- Breathing exercises and physical therapy improve lung function.
3. Lifestyle Modifications
- Quitting smoking, maintaining a healthy diet, and staying active.
4. Lung Transplantation
- Considered in severe cases where other treatments fail.
Living with Pulmonary Fibrosis
- Regular medical checkups are essential.
- Emotional and psychological support (support groups, counseling).
- Manage symptoms with prescribed therapies and lifestyle changes.
FAQs on Pulmonary Fibrosis
1. Is pulmonary fibrosis a terminal disease?
Pulmonary fibrosis is a progressive disease, but early diagnosis and treatment can improve life expectancy and quality of life.
2. Can pulmonary fibrosis be reversed?
No, lung scarring cannot be reversed, but treatments can slow disease progression and manage symptoms.
3. How long can a person live with pulmonary fibrosis?
Life expectancy varies, but many patients live for several years with proper treatment.
4. Is pulmonary fibrosis contagious?
No, pulmonary fibrosis is not infectious and cannot be spread from person to person.
5. Does smoking cause pulmonary fibrosis?
Smoking increases the risk of lung diseases, including pulmonary fibrosis.
6. Can exercise help with pulmonary fibrosis?
Yes, pulmonary rehabilitation and breathing exercises can help improve lung function.
7. What foods should I eat if I have pulmonary fibrosis?
A balanced diet rich in fruits, vegetables, lean protein, and healthy fats supports overall health.
8. Is there a cure for pulmonary fibrosis?
Currently, there is no cure, but treatments can help manage symptoms and slow disease progression.
9. Are there clinical trials for pulmonary fibrosis?
Yes, ongoing research and clinical trials aim to develop new treatments.
10. Can air pollution worsen pulmonary fibrosis?
Yes, air pollutants and environmental toxins can aggravate lung conditions.
Conclusion
Pulmonary fibrosis is a challenging condition, but with proper understanding and management, patients can lead fulfilling lives. Early diagnosis, effective treatments, and lifestyle changes are key to slowing disease progression. If you or a loved one is experiencing symptoms, seek medical advice promptly. Stay informed, stay proactive, and remember that support is available for those affected by pulmonary fibrosis.