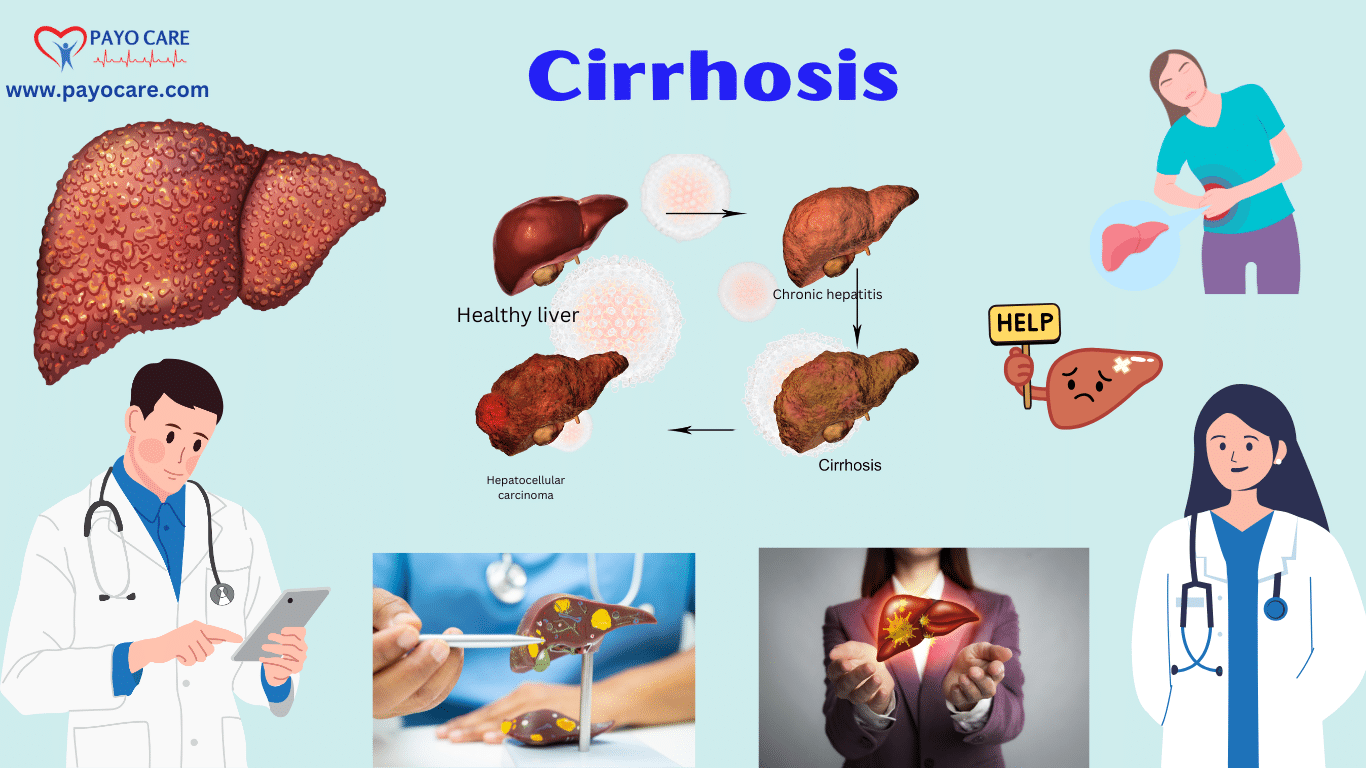
Cirrhosis is a chronic liver disease characterized by the gradual replacement of healthy liver tissue with scar tissue (fibrosis). This scarring disrupts liver function, leading to serious health complications. Cirrhosis is a progressive condition that worsens over time, eventually leading to liver failure if left untreated.
Liver disease is a significant global health burden, with millions of people affected each year. The major causes of cirrhosis include long-term alcohol abuse, viral hepatitis, and non-alcoholic fatty liver disease (NAFLD). Early detection and appropriate treatment can slow or even stop its progression. This article will explore the different types of cirrhosis, its causes, symptoms, prevention, diagnosis, and treatment options.
Types of Cirrhosis
Cirrhosis can be classified based on its cause and how it affects the liver. Some of the common types include:
1. Alcoholic Cirrhosis
This type of cirrhosis occurs due to prolonged and excessive alcohol consumption. The liver metabolizes alcohol, but excessive drinking causes inflammation and damage to liver cells, eventually leading to fibrosis and cirrhosis. It is the most common type of cirrhosis in many countries.
2. Post-Hepatic (Viral) Cirrhosis
Chronic viral infections such as hepatitis B and hepatitis C can cause liver damage over time. The persistent inflammation associated with these infections leads to scarring and cirrhosis.
3. Non-Alcoholic Fatty Liver Disease (NAFLD) Cirrhosis
NAFLD is a condition where excess fat accumulates in the liver, often due to obesity, diabetes, or metabolic disorders. When NAFLD progresses to non-alcoholic steatohepatitis (NASH), it causes inflammation and scarring, leading to cirrhosis.
4. Biliary Cirrhosis
This type occurs when the bile ducts, responsible for carrying bile from the liver to the small intestine, become damaged. There are two major forms:
- Primary Biliary Cholangitis (PBC): An autoimmune condition where the body’s immune system attacks the bile ducts.
- Secondary Biliary Cirrhosis: Caused by prolonged blockage of bile ducts due to gallstones, tumors, or cystic fibrosis.
5. Cardiac Cirrhosis
This type of cirrhosis is caused by chronic right-sided heart failure, which leads to blood congestion in the liver. This congestion damages liver cells over time, leading to fibrosis and cirrhosis.
6. Genetic or Metabolic Cirrhosis
Some genetic conditions, such as hemochromatosis (iron overload) and Wilson’s disease (copper accumulation), can lead to liver damage and cirrhosis. These disorders interfere with normal liver metabolism, causing toxic accumulation of metals and scarring.
Causes of Cirrhosis
Several factors can contribute to liver damage and the development of cirrhosis. The most common causes include:
1. Chronic Alcohol Abuse
Excessive alcohol consumption over many years is one of the leading causes of cirrhosis. The liver metabolizes alcohol, but in large amounts, it becomes overwhelmed, leading to inflammation, fatty liver, and scarring.
2. Chronic Viral Hepatitis (Hepatitis B, C, and D)
Viral hepatitis is a major cause of cirrhosis worldwide. Hepatitis B and C infections cause chronic liver inflammation, leading to scarring and cirrhosis over time.
3. Non-Alcoholic Fatty Liver Disease (NAFLD)
NAFLD is linked to obesity, diabetes, high cholesterol, and metabolic syndrome. It can progress to NASH, which causes inflammation and fibrosis, eventually leading to cirrhosis.
4. Autoimmune Diseases
Conditions such as autoimmune hepatitis cause the immune system to attack liver cells, leading to chronic inflammation and scarring.
5. Genetic Disorders
Inherited metabolic disorders like hemochromatosis (excess iron absorption) and Wilson’s disease (copper accumulation) can cause cirrhosis.
6. Bile Duct Diseases
Obstruction or inflammation of the bile ducts, as seen in primary biliary cholangitis and primary sclerosing cholangitis, can lead to liver scarring and cirrhosis.
7. Long-Term Drug or Toxin Exposure
Certain medications, toxic substances, and industrial chemicals can cause liver damage over time, leading to cirrhosis.
8. Chronic Heart Failure
Chronic right-sided heart failure can lead to congestion in the liver, damaging liver cells and causing cirrhosis.
Symptoms of Cirrhosis
In the early stages, cirrhosis may not cause noticeable symptoms. However, as the disease progresses, symptoms become more apparent.
Early Symptoms:
- Fatigue
- Weakness
- Loss of appetite
- Nausea
- Weight loss
- Mild abdominal pain or discomfort
Advanced Symptoms:
- Jaundice (yellowing of the skin and eyes)
- Edema (swelling in the legs, ankles, and feet)
- Ascites (fluid buildup in the abdomen)
- Itchy skin due to bile buildup
- Easy bruising and bleeding due to impaired liver function
- Dark urine and pale stools
- Mental confusion (hepatic encephalopathy) due to toxin buildup
- Spider-like blood vessels (spider angiomas) on the skin

Prevention of Cirrhosis
Although some causes of cirrhosis are unavoidable, many cases can be prevented by adopting a healthy lifestyle and managing risk factors.
1. Limit Alcohol Consumption
Avoid excessive drinking or quit alcohol entirely if you have liver disease.
2. Get Vaccinated Against Hepatitis
Hepatitis B and C infections can lead to cirrhosis. Getting vaccinated and practicing safe behaviors can reduce the risk.
3. Maintain a Healthy Diet
Eating a balanced diet rich in fruits, vegetables, whole grains, and lean proteins can prevent fatty liver disease.
4. Maintain a Healthy Weight
Obesity increases the risk of NAFLD. Regular exercise and a healthy diet can help prevent liver damage.
5. Avoid Risky Behaviors
Avoid sharing needles, practice safe sex, and be cautious with tattoos or piercings to prevent hepatitis infections.
6. Manage Chronic Health Conditions
Control diabetes, high cholesterol, and hypertension, as these conditions can contribute to liver disease.
Diagnosis of Cirrhosis
Cirrhosis is often diagnosed through a combination of medical history, physical examination, imaging tests, and laboratory tests.
1. Blood Tests:
- Liver function tests (ALT, AST, bilirubin)
- Complete blood count (CBC)
- Blood clotting tests
- Albumin levels (low levels indicate liver dysfunction)
- Tests for hepatitis and autoimmune markers
2. Imaging Tests:
- Ultrasound: First-line imaging test to detect liver abnormalities.
- CT Scan/MRI: Provides detailed liver images to assess fibrosis and complications.
- FibroScan: A special ultrasound that measures liver stiffness (a sign of fibrosis).
3. Liver Biopsy:
A small sample of liver tissue is examined under a microscope to confirm cirrhosis and determine its severity.
Treatment of Cirrhosis
There is no cure for cirrhosis, but treatment can slow its progression, manage symptoms, and prevent complications.
1. Lifestyle Changes:
- Stop alcohol consumption immediately.
- Follow a liver-friendly diet with low sodium and high fiber.
- Exercise regularly to maintain a healthy weight.
2. Medications:
- Antiviral drugs for hepatitis B or C.
- Medications to reduce portal hypertension and prevent variceal bleeding.
- Diuretics to remove excess fluid from the body.
- Lactulose to manage hepatic encephalopathy.
3. Procedures & Surgeries:
- Endoscopic Treatments: To stop internal bleeding from varices.
- Liver Transplant: The only definitive treatment for end-stage cirrhosis.
Article Covers
- Cirrhosis types and causes
- Symptoms of cirrhosis
- How to prevent cirrhosis
- Diagnosing cirrhosis
- Cirrhosis treatment options
- Alcoholic liver disease and cirrhosis
- Non-alcoholic fatty liver disease (NAFLD)
- Liver cirrhosis complications
- Cirrhosis diet and lifestyle tips
- Early signs of liver damage
Conclusion
Cirrhosis is a serious condition that requires early diagnosis and proper management to prevent complications. By understanding its types, causes, symptoms, and treatment options, individuals can take proactive steps to protect their liver health. If you suspect you have cirrhosis or are at risk, consult a healthcare professional for accurate diagnosis and personalized treatment.