Sleep apnea is a common but serious sleep disorder characterized by repeated interruptions in breathing during sleep. These interruptions, known as apneas, can last for a few seconds to a minute and occur dozens or even hundreds of times per night. Sleep apnea disrupts sleep quality, leading to daytime fatigue, cognitive impairment, and an increased risk of cardiovascular and metabolic disorders. Understanding the types, causes, symptoms, prevention, diagnosis, and treatment options for sleep apnea is essential for managing the condition and improving overall health and well-being.
Types of Sleep Apnea
There are three main types of sleep apnea:
1. Obstructive Sleep Apnea (OSA)
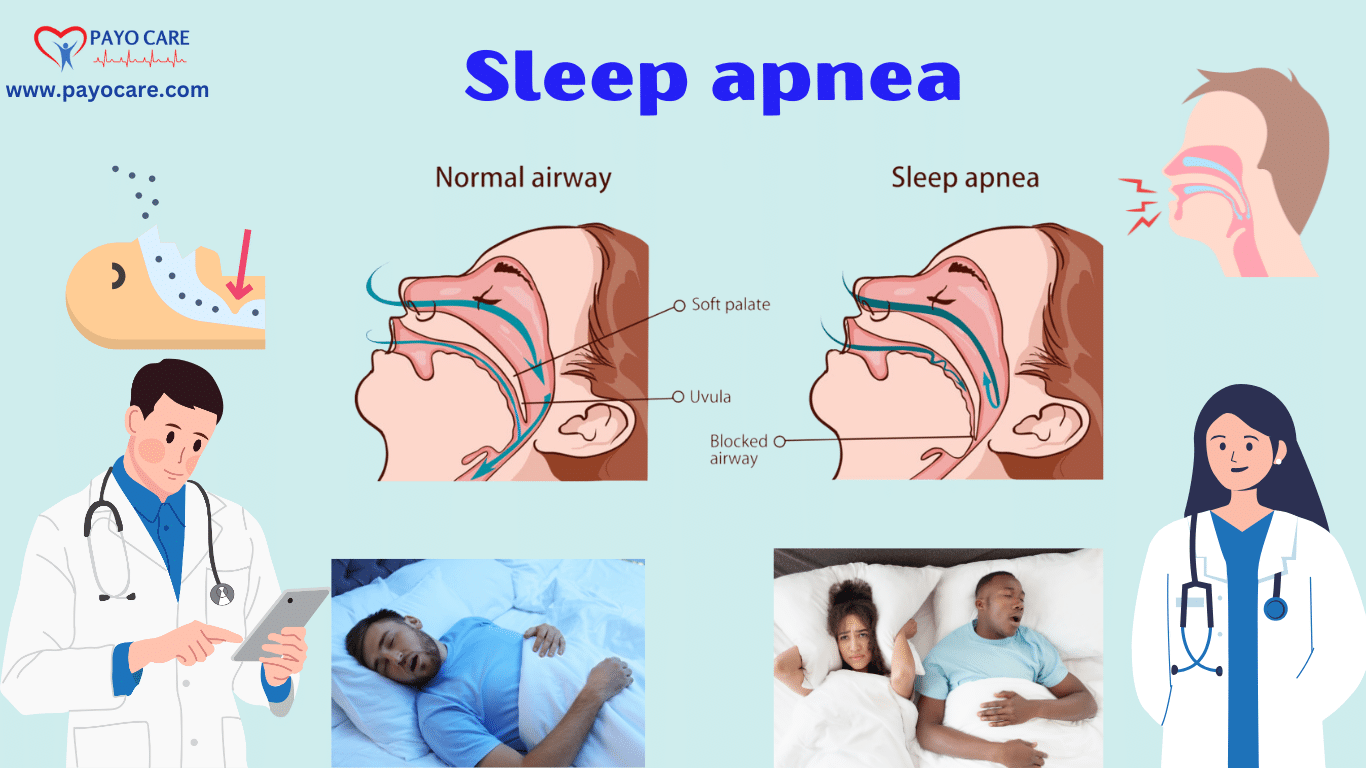
OSA is the most common type of sleep apnea. It occurs when the muscles in the throat relax excessively during sleep, leading to a blocked airway. This causes temporary breathing pauses and reduced oxygen levels in the blood.
2. Central Sleep Apnea (CSA)
CSA is a less common form of sleep apnea and occurs when the brain fails to send proper signals to the muscles that control breathing. Unlike OSA, there is no physical obstruction in the airway; instead, it is a neurological issue.
3. Complex Sleep Apnea Syndrome
Also known as treatment-emergent central sleep apnea, this condition occurs when a person has both obstructive sleep apnea and central sleep apnea. It often develops when someone with OSA is treated with continuous positive airway pressure (CPAP) therapy but later exhibits central sleep apnea symptoms.
Causes of Sleep Apnea
Several factors contribute to the development of sleep apnea, depending on the type:
Causes of Obstructive Sleep Apnea (OSA):
- Obesity: Excess weight can lead to fat deposits around the upper airway, increasing the risk of obstruction.
- Enlarged Tonsils or Adenoids: This is a common cause in children.
- Structural Issues: A narrow airway, large tongue, or receding jaw can contribute to OSA.
- Smoking and Alcohol Use: These can cause inflammation and relaxation of throat muscles, worsening apnea.
- Nasal Congestion: Chronic nasal congestion can restrict airflow, increasing the likelihood of OSA.
- Family History: A genetic predisposition can make some individuals more prone to OSA.
Causes of Central Sleep Apnea (CSA):
- Neurological Conditions: Disorders like stroke, brain infections, or Parkinson’s disease can impair brain signals to breathing muscles.
- Heart Failure: Congestive heart failure can lead to CSA by disrupting normal breathing patterns.
- Certain Medications: Opioids and other drugs that depress the central nervous system can cause CSA.
- High Altitudes: Living or traveling to high-altitude regions can trigger CSA due to lower oxygen levels.
Symptoms of Sleep Apnea
The symptoms of sleep apnea vary depending on the severity and type. Some common symptoms include:
Nighttime Symptoms:
- Loud snoring (especially in OSA)
- Gasping or choking during sleep
- Pauses in breathing observed by a partner
- Frequent awakenings or restless sleep
Daytime Symptoms:
- Excessive daytime sleepiness
- Morning headaches
- Difficulty concentrating
- Irritability and mood swings
- Dry mouth or sore throat upon waking

Prevention of Sleep Apnea
While some risk factors for sleep apnea cannot be controlled, lifestyle changes can significantly reduce the risk:
- Maintain a Healthy Weight: Losing excess weight can reduce fat deposits around the airway.
- Avoid Alcohol and Sedatives: These substances relax throat muscles and can worsen apnea.
- Quit Smoking: Smoking increases inflammation and fluid retention in the airway.
- Sleep on Your Side: Sleeping on your back can cause the tongue and soft tissues to block the airway.
- Treat Nasal Congestion: Using nasal sprays or humidifiers can improve airflow.
- Exercise Regularly: Regular physical activity can improve overall respiratory function and aid weight loss.
Diagnosis of Sleep Apnea
A medical evaluation is necessary for an accurate diagnosis. The following tests are commonly used:
1. Polysomnography (Sleep Study)
A comprehensive sleep study conducted in a sleep lab. It monitors brain waves, oxygen levels, heart rate, breathing patterns, and body movements during sleep.
2. Home Sleep Apnea Test (HSAT)
A simplified version of polysomnography that can be performed at home. It measures oxygen levels, airflow, and breathing patterns.
3. Physical Examination and Medical History
Doctors assess symptoms, risk factors, and perform physical examinations, such as checking airway structure and BMI.
Treatment of Sleep Apnea
1. Lifestyle Modifications
For mild cases of sleep apnea, lifestyle changes can be effective:
- Weight Loss: Reducing excess weight can improve airway obstruction.
- Positional Therapy: Sleeping on the side instead of the back can help prevent airway collapse.
- Avoiding Triggers: Alcohol, smoking, and sedatives should be minimized.
2. Continuous Positive Airway Pressure (CPAP)
CPAP therapy is the most effective treatment for moderate to severe OSA. It involves wearing a mask connected to a machine that delivers constant air pressure to keep the airway open.
3. Bi-Level Positive Airway Pressure (BiPAP)
For those who cannot tolerate CPAP, BiPAP delivers different pressure levels for inhalation and exhalation, making breathing easier.
4. Oral Appliances
Mouthpieces designed to reposition the jaw and tongue can help keep the airway open, especially for mild to moderate OSA.
5. Surgery
In severe cases, surgical interventions may be necessary:
- Uvulopalatopharyngoplasty (UPPP): Removes excess tissue in the throat.
- Tonsillectomy: Removes enlarged tonsils that block the airway.
- Nasal Surgery: Corrects structural issues like a deviated septum.
- Implants: Devices like Inspire therapy stimulate airway muscles to prevent collapse.
6. Medications
While there are no specific drugs for sleep apnea, medications for underlying conditions (such as heart failure or neurological disorders) can help manage symptoms.
7. Adaptive Servo-Ventilation (ASV)
This is an advanced therapy used for CSA. It adjusts airflow based on breathing patterns and can be more effective than CPAP in certain cases.
- What is Sleep Apnea?
Sleep apnea is a sleep disorder in which breathing repeatedly stops and starts during sleep. This can lead to poor sleep quality and other health complications if left untreated. - What are the common symptoms of Sleep Apnea?
Symptoms include loud snoring, gasping or choking during sleep, excessive daytime sleepiness, difficulty concentrating, morning headaches, and irritability. - What causes Sleep Apnea?
The most common type, obstructive sleep apnea (OSA), occurs when throat muscles relax and block the airway. Other factors include obesity, smoking, alcohol consumption, and a family history of the condition. - How is Sleep Apnea diagnosed?
Diagnosis typically involves a sleep study (polysomnography) conducted in a sleep lab or at home. This test monitors breathing, oxygen levels, and brain activity during sleep. - What are the treatment options for Sleep Apnea?
Treatments include lifestyle changes (weight loss, avoiding alcohol, and sleeping on your side), the use of a CPAP (continuous positive airway pressure) machine, oral appliances, and, in severe cases, surgery to remove airway obstructions.
Conclusion
Sleep apnea is a serious sleep disorder that can have significant health consequences if left untreated. By understanding the types, causes, symptoms, prevention strategies, diagnostic methods, and treatment options, individuals can take proactive steps to manage the condition and improve their quality of life. Early diagnosis and appropriate treatment are crucial for reducing the risk of complications and ensuring restful, restorative sleep. With advances in medical technology and a focus on lifestyle modifications, there is hope for effective management and better outcomes for those affected by sleep apnea.